Key Points:
- What is the prevalence of rotator cuff pathology?
- Rotator cuff tendinopathy is the most common form of shoulder pain (1)
- What is Rotator Cuff Tendinopathy and Associated Rotator Cuff Tearing?
- Rotator cuff tendinopathy is a degenerative breakdown of the rotator cuff tendons (14)
- How Does Tendinopathy Occur?
- Tendinopathy occurs to the tendon when the stress applied to the tendon is greater then it's ability to recover (14)
- How Do Rotator Cuff Tears Occur?
- Rotator cuff tears are most commonly a continuation of tendinopathy where the tendon begins to tear and progressively worsens over time (14)
- What Are the Causes (Mechanism of injury) of Rotator Cuff injuries?
- Rotator cuff tears happen for a variety of reasons including age, overuse, overload, trauma, specific acromion shapes and abnormal shoulder / shoulder blade mechanics. (24)
- What is the Clinical Presentation of this Injury?
- Reduced shoulder function, pain (radiating to the lateral mid‐humerus or anterolateral acromion), stiffness, weak external rotators and supraspinatus (4)
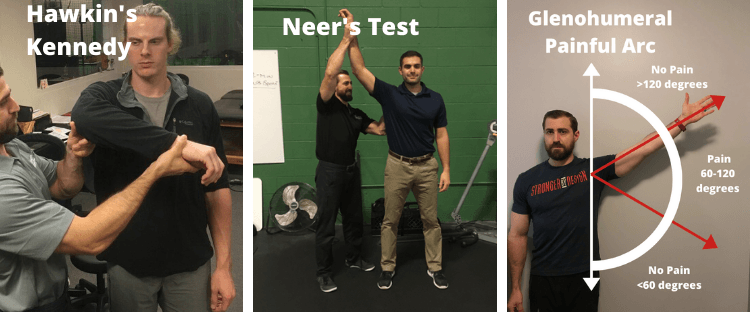
- Positive special tests meant to provoke symptoms (Hawkin's Kennedy, Neer's) (4)
- What Are The Expectations for Recovery with Tendinopathy and Rotator Cuff Tears?
- Most people have improvement in pain and function with conservative treatment including physical therapy for tendinopathy and rotator cuff tears (47)
- When is surgery indicated for rotator cuff tears?
- Acute (traumatic) tears >1 cm (48)
- Chronic (degenerative) full thickness tears >1cm and patient age <60 years old (48)
- Tears >1 cm that have failed conservative treatment (48)
- What are the outcomes from rotator cuff repair?
- Outcomes of rotator cuff repair are generally good with up to 90% of patients being happy with the outcome at 6 months (58)
Shoulder pain is easily one of the most common issues strength and fitness athletes face in the gym on a regular basis. It's also one of the most common issues I treat on a regular basis as a physical therapist. Because of this I wanted to create a fully comprehensive guide on rotator cuff pathology to help both rehabilitation and fitness professionals work with this population. More specifically, I wanted to make a guide detailing rotator cuff tears, tendinopathy and subacromial impingement syndrome since it's just such a common problem. Buckle up because this is going to be a long read.
What is the Prevalence of Rotator Cuff Pathology?
Rotator cuff tendinopathy is the most common form of shoulder pain (1). It is often times lumped into the same diagnosis of subacromial impingement syndrome although as we'll discuss later this is not always totally true. It's the 3rd most common musculoskeletal issue that causes people to consult their primary care physician. Just about 1% of all adults will talk to their physician about shoulder pain which includes rotator cuff issues every year (1).
Prevalence in the General Population
Between 16 and 26% of a general population will report shoulder pain at any given time (1). It is believed that the majority of this pain is coming from the cuff, either from some sort of tendinopathy, impingement or tear. So ya, rotator cuff pathology is actually fairly common
Cuff tears are also more common as we age (10).
- 51.8% of people aged 60-69 have a partial thickness rotator cuff tear (14.4% had a full thickness tear)
- 61.8% of people aged 70-79 have a partial thickness rotator cuff tear (26.3% had a full thickness tear)
- 72.5% of people aged 80-89 have a partial thickness rotator cuff tear (29% had a full thickness tear)
Based on these stats you'd be luckly to get through life without a rotator cuff tear. However, rotator cuff tearing is not as common in younger folks (<30 years old). (11) In fact, rotator cuff tears don't commonly start showing up in people until they're over 40 years old. (11) Keep in mind that tendinopathy is the degenerative precursor to tears and occurs much earlier in your shoulder's lifespan in comparison to tears.
Prevalence in Athletes
With that being said, your activity will also dictate the amount of rotator cuff damage you take over time. One super obvious example is in baseball players (especially pitchers) who obviously perform a lot of throwing and subsequently stress the heck out of their rotator cuff. 21-52% of asymptomatic (throwers without pain - more on this later) major league baseball pitchers have a rotator cuff tear. (12)
Studies in little league baseball players (age 10-12) show that 17% of players had a partial thickness rotator cuff tear. (12) In this same study they were 8 times more likely to have rotator cuff issues on the throwing side then the non-throwing side. (12) These abnormalities were correlated with year-round play and single-sport specialization. (12)
Side Note: These players were even compliant with the Little League throwing guidelines.
So yup, the more often we use (and abuse) our shoulders, the more likely we are to end up with rotator cuff issues.
Prevalence in Strength and Fitness
Now that we know that rotator cuff injuries are more common in an older general population and in overhead athletes like pitchers, how about with strength and fitness athletes? Well, it's also a pretty common injury there too...
Among CrossFit (TM) participants, the shoulder routinely ranks among the top 3 most injured areas and in some studies is reported as the most injured area during participation. (3, 13) In the same study shoulder injuries occurred at a rate of ~2 injuries per 1,000 hours of participation. (13) So if we do the math that means if you train in CrossFit (TM) 5 days per week for 60 minutes that means you're likely to get 1 shoulder injury for every 2 years of participation. (That's assuming you train in the gyms where they recorded this data)
Powerlifting and Olympic Weightlifting is also pretty similar. Depending on the study you read the shoulder will also rank in the top 3 coming in neck and neck with lower back and knee injuries (3).
Also keep in mind that in these studies they did not say this was an injury to the rotator cuff. Most studies used survey data asking people where they got hurt. I'm just assuming that a chunk of these injuries were probably from some rotator cuff irritation although I'm sure the cuff wasn't the only issue.
I have personally worked with several competitive powerlifters, CrossFit (TM) athletes and olympic weightlifters who have had rotator cuff tears well before the age of 30. Atleast to me it stands to reason that these activities can also create rotator cuff pathology like in other overhead sports. To what degree, I don't think we have any research about this just yet.
Regardless, if you've been training in any of those sports yourself, regularly hit the gym hard yourself, or work with athletes in this realm then sooner or later you'll probably be experiencing this. It just happens and it's probably related to the amount of stress we throw at our joints.
What is Rotator Cuff Tendinopathy and Associated Rotator Cuff Tearing?
Relevant Anatomy
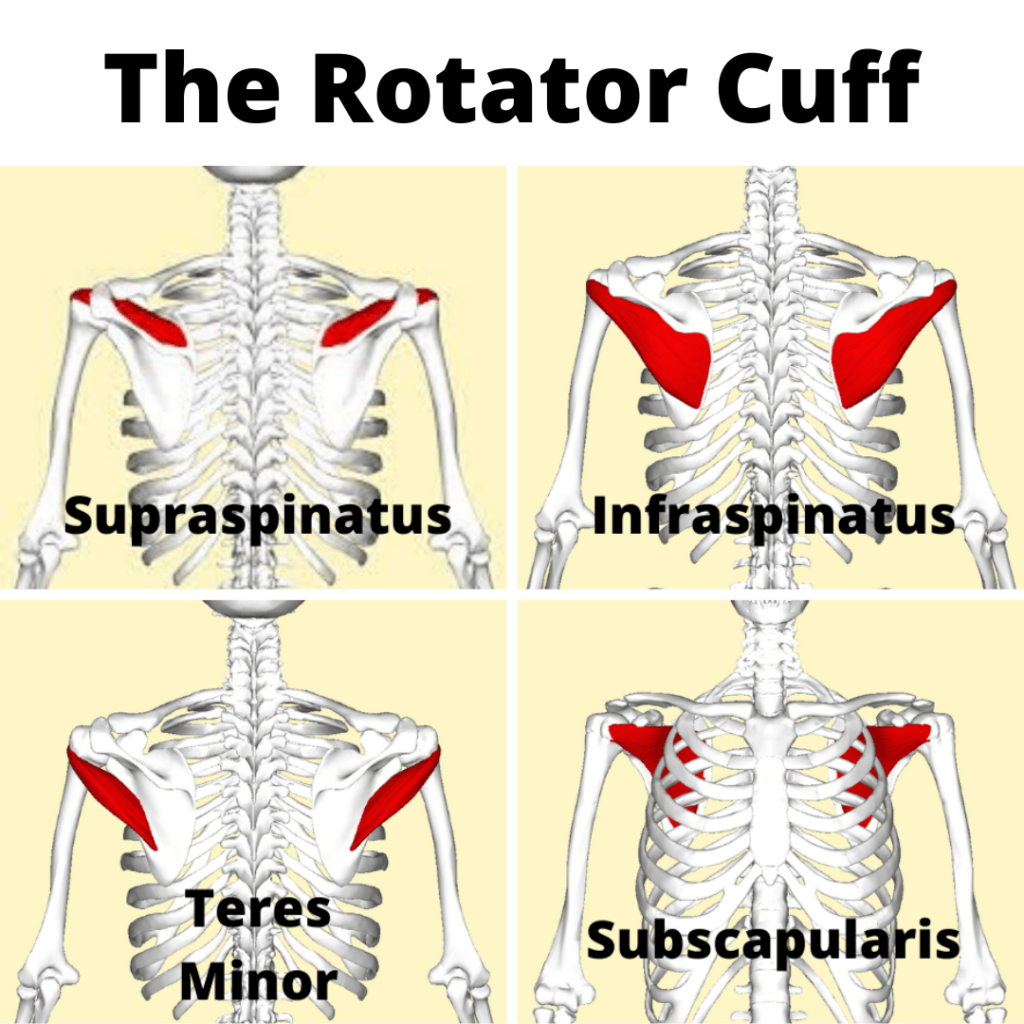
The rotator cuff consists of 4 muscles (supraspinatus, infraspinatus, teres minor, subscapularis) that help to control motion within the glenohumeral joint.
Think of starting a bench press program that has you pressing 5 days per week when you're only accustomed to pressing 1 time per week.
Tendinitis vs. Tendinosis
These issues were formerly known as rotator cuff “tendinitis”. The “itis” portion of tendinitis generally refers to an inflammatory condition. We used to think that the tendon becomes painful because of inflammation in the area.
What we’ve found over the course of time and with research is that this condition is not mainly inflammatory in nature but more of a degenerative (wear and tear) condition (7). Basically, with excessive stress over the course of time the tendon attempts to adapt to the stress of training. The tendon goes through changes because of this stress and can sometimes become painful. This is referred to as “osis” or the “opathy” found at the end of rotator cuff tendin-opathy.
“itis” vs “osis”
Side Note: Research in rotator cuff tendinopathy is mixed in terms of how much inflammation is evident in the degenerative process. There are inflammatory markers present during tendinopathy in the rotator cuff but the process is different then a normal inflammatory reaction. (4)
Tendons perform similarly to springs in the sense that they store and release energy. High performance activities like jumping and weight training require the tendons to store and release energy just like a spring does (8). The better tendons store and release energy the better we perform these activities (8).
If we perform too much tendon intensive movement, or have insufficient rest between bouts of tendon intensive activity we don’t allow the remodeling process that normally occurs after stressing a tendon (7). This can induce pathology and changes in the tendon’s mechanical properties (7). This is what we refer to as "tendinopathy" or "tendinosis".
Tendinopathy in the rotator cuff can also be also be caused by a lack of stress as well. Insufficient stimulus can cause tendons to degenerate just as too much stress does. (7)
What Tendinopathy Does to Tendons
In tendinopathy the collagen make-up of the tendons become disorganized in comparison to it’s normal longitudinal alignment. (7) The collagen matrix is thicker and weaker with more water, more immature and cartilage-like matrix proteins. (5) The tendon cells are rounder, more numerous, and show evidence of oxidative damage and more apoptosis (cell death) then usual. (5)
Side Note: Thickening of tendons is a common problem associated with tendinopathy of the achilles. However, the rotator cuff thickens in some individuals but can also shrink in others. The thickening phenomenon of tendinopathy is not cut and dry in the rotator cuff. (4)
Over the course of time and with sufficient stress (or lack of stress) the tendon can continue to worsen and progressive tearing occurs. There's how the majority of rotator cuff tears occur. (7) (Rotator cuff tears can also occur due to trauma as well but are less common)
Risk Factors for Developing Rotator Cuff Tendinopathy
Factors that increase your risk of getting rotator cuff tendinopathy are: (35)
- Age above 50 years
- Diabetes
- Overhead activities (as an occupation or sport)
- Dyslipidemia (High Cholesterol) (55)
So your risk of tendinopathy goes up with age, chronic blood sugar and cholesterol levels.
How Does Tendinopathy Occur?
Stages of Tendon Pathology
Our best guess as to how tendons progress from healthy to tendinosis to tears is via a continuum model. (14) This consists of 3 stages:
- Reactive Tendinopathy
- Tendon Dysrepair
- Degenerative Tendon
1: Reactive Tendinopathy (14)
This reactive stage we see clinically in a tendon that's been acutely overloaded. Again, think about the young gentlemen that just decided to bench press 5 days per week when formerly being used to benching once per week.
Folks who aren't prepared for a given activity and then head first into a new training program are especially susceptible to this. Reactive tendinopathy is generally seen more in younger individuals. Although this is usually seen with acute overload, this can also happen with direct trauma to the tendon as well.
2: Tendon Dysrepair (14)
After the reactive stage comes tendon dysrepair. In this stage the tendon is attempting to heal. There is an increase in chondrocytic cells and myofibroblasts which results in an increase in protein production (proteoglycans and collagen). The increased number of proteoglycans results in a separation of the normal collagen cells which leads to the disorganization of the tissue matrix. There also may be an increase in vascularity and neuron growth in the tendon as well at this stage.
Side Note: It is theorized that this increase in nerve supply would correlate with increased pain but this isn't always the case in the rotator cuff (4)
3: Degenerative Tendon (14)
The degenerative tendon stage is exactly what it sounds like. Areas of cell death become more and more apparent leaving whole areas of acellularity. Large areas of the matrix are disorganized and filled with vessels. Areas that were filled with collagen are replaced with matrix breakdown products. Under a microscope you'll see large "islands" of degenerative tendon mixed with areas of normal tendon. This is also the stage where where you'll start seeing tearing of the rotator cuff tendons as well. (7)
How Do Rotator Cuff Tears Occur?
Most rotator cuff tears begin as a continuation of the degeneration process. Traumatic tears are much less common and more prevalent in younger folks.
Which Tendons are Most Commonly Torn?
The supraspinatus tendon is widely regarded as the most commonly injured tendon and where the majority of degenerative rotator cuff tears begin, particularly 9-10 mm posterior to the biceps tendon. (16) This evidence is mixed and some authors report the infraspinatus is the most common place for tears to begin. (15) Either way, cuff tears probably begin somewhere between these two muscles. Tendinopathy as described earlier is a precursor to degenerative cuff tears and our research shows that a tendon with more tendinopathy (particularly thickening) is more likely to tear over time. (19)
Where in the Tendon are Tears Located?
Tears to the rotator cuff tendons can occur in 1 of 3 areas. (4) The first is known as articular sided tears. Articular sided tears occur on the bottom of the tendon which is closest to the joint (articulation). (4) The second is a bursal sided tear. Bursal sided tears occur at the top of the tendon closest to the bursa. (4) Mid-substance tears are the 3rd type of tear and they occur in the inner substance of the tendon. (4)
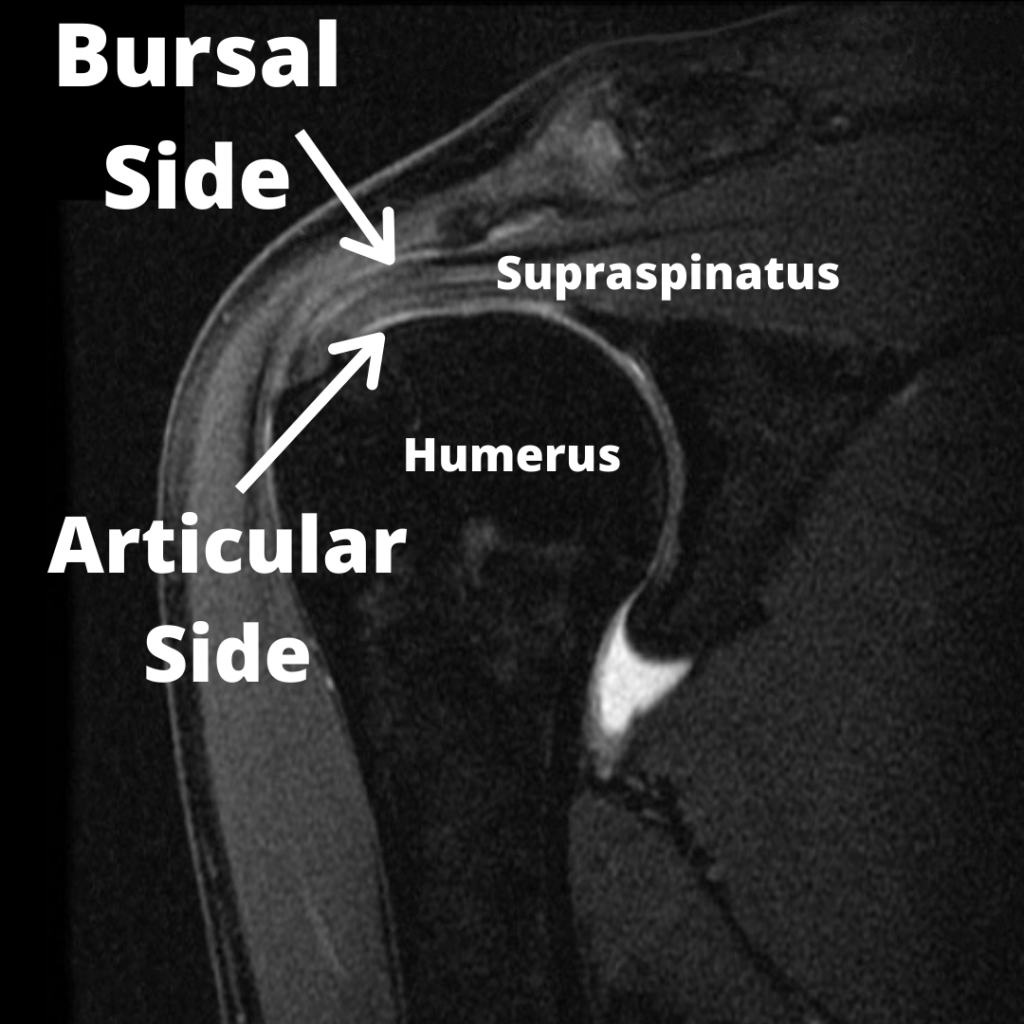 Image Source, License, Attribution: RSatUSZ / CC BY-SA - edited by Fitness Pain Free LLC
Image Source, License, Attribution: RSatUSZ / CC BY-SA - edited by Fitness Pain Free LLCThe location of the tear can be important in the treatment and mechanism of injury so more on this later...
Full Thickness vs. Partial Thickness and Grading Tear Severity
Chronic degenerative rotator cuff tears start as "partial thickness" tears and progress over time to "full thickness" tears. Partial thickness tears perfectly describe what they are, only a partial tearing of the rotator cuff. The severity of the tear is also defined by what percentage of the tendon is torn (25% vs. 50% vs. 75%). (19) Full thickness tears are also appropriately named and describe a fully torn tendon. When full thickness tears pull away from their insertion on the humerus they are known as "retracted" tears.
Do Rotator Cuff Tears Heal Over Time?
Unfortunately, rotator cuff tears most commonly do NOT heal over the course of time (19). They generally progressively worsen as we age. (18, 19) How fast they progress over time varies from person to person. Keener et al. studied 224 shoulders with asymptomatic cuff tears over the course of 2.8 years and found that tears enlarged in 49% of the population. (18) Tear size is one variable that dictates the speed of rotator cuff disease progression. (20) (i.e. Larger tears get larger more quickly then smaller tears). For example:
- Progression rates for partial thickness tears <50% torn are 14% over two years
- Progression rates for partial thickness tears >50% are 55% over two years
Research is mixed in terms of what variables will increase your risk of cuff tear progression. Here are some commonly cited ones (19):
- Having a tear in your dominant hand
- The development of pain (in asymptomatic tears)
- Cuff muscle degeneration (atrophy)
- Follow up >18 months (so in other words, more time between MRIs)
- Advanced age
- Prior trauma
- More fatty muscle infiltration
- Having a full thickness tear vs. a partial thickness tear
- Smoking
So ya, trying to figure out if your client's rotator cuff injury is going to get worse over the course of time is really tough to figure out.
As the tear progressively gets larger over time and progresses from a partial to full thickness tear, the rotator cuff muscles can start to be replaced with fat in a process known as "fatty infiltration". (17, 18) As tearing progresses, the amount of fatty infiltration increases and more tendons become torn (supraspinatus --> infraspinatus --> subscapularis etc). (18)
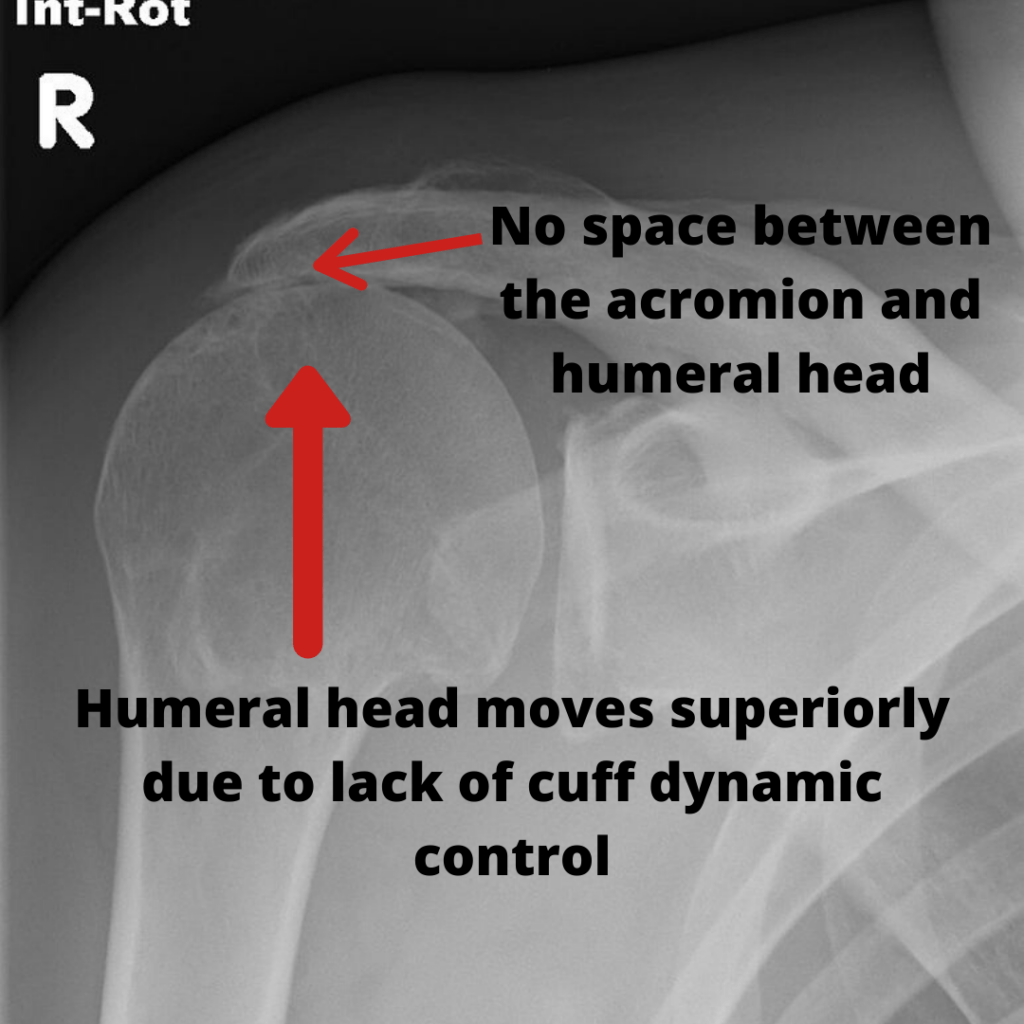
Once enough tendon damage occurs, the rotator cuff can no longer stabilize the humeral head in the glenoid and superior humeral head migration occurs. (18) This is at the very end stages of rotator cuff degeneration and damage.
Understanding Rotator Cuff Pathology and Pain
Now, given all of these tendon changes you'd assume that this means you'll have pain as well right? Well, not exactly.
Hold your horses, so having these tendon issues doesn’t automatically mean we’ll have pain?
No, generally only about 20% of people with radiographic evidence (MRI or Ultrasound) of tendinopathy actually have pain (9). This means that around 80% of people with tendinopathy have no pain at all (9).
In other words, tendons in your body that take stress over time are likely to develop some tendinopathy. We know this occurs in sports where certain tendons are predictably stressed (Think patellar tendinopathy in basketball players, cuff tendiopathy in pitchers and tennis elbow in tennis players) (7).
This doesn’t mean that you’ll develop pain but you ARE more likely to develop pain then someone without tendinopathy (7).
I’ll repeat this because it’s a little confusing. People with tendinopathy diagnosed with an MRI or ultrasound don’t always have pain but are at an increased risk of developing pain at some point in the future.
The same thing goes for rotator cuff tears which can occur without any symptoms as well. (6) In studies of general populations with cuff tears only about 1/3 of these folks had any symptoms at all. (6)
So ya, most people with a rotator cuff tear have no idea they have a rotator cuff tear...
However, the larger the cuff tear was the more likely the shoulder was to be symptomatic (painful). (10) Pain intensity is also reported to be greater in people with larger cuff tears. (10) Patients with more pain also tended to have more tendinopathy then those without it. In a study of senior (>60 years old) athletes the odds of having shoulder pain was eight times greater in those athletes with any rotator cuff damage as compared with those without any rotator cuff damage. (36) Lastly, partial thickness tears are often less symptomatic then full thickness tears. (20)
So at the end of the day having pathology like tendinopathy and tears will increase the likelihood of having pain and the worse the pain is, generally the worse the damage is as well.
How Do Rotator Cuff Tears Occur?
The creation of tendinopathy and tears is a topic of hot debate. 30 years ago we actually thought we had a pretty cut and dry answer to this question. Now we know this issue is a bit more complex then previously thought and we've actually changed our minds a bit in terms of what creates these tears. There are two main types of factors that contribute to the formation and worsening of rotator cuff problems. These are intrinsic and extrinsic factors:
Intrinsic Factors (4, 24):
- Aging
- Microvascular Blood Supply
- Alteration in Tendon Matrix on Mechanical Properties Through Overload and Overuse
- Trauma
Extrinsic Factors (4, 24):
- Acromial Shape
- Acromial Slope / Angle
- Acromioclavicular (AC) Joint Arthritic Changes
- Abnormal Humeral Kinematics
- Abnormal Scapular Kinematics
- Posture
- Soft Tissue Tightness
Intrinsic Factors
It has become more and more evident over the course of time that intrinsic factors are more responsible for rotator cuff tears then extrinsic factors. (4) (More on this later)
1: Aging
Unfortunately as we age several processes occur that will ultimately lead to degeneration of our tendons. This can also help explain why the occurrence of rotator cuff tears is so much more common as we age. As we age our tendons are negatively affected by processes like calcification and fibrovascular proliferation. (4,24) Age also creates decreased tensile loading capability and decreased elasticity within our tendons. (4,24) Unfortunately we really can't really do much about reversing or stopping the aging process.
2: Microvascular Blood Supply
It is theorized that a lack of blood supply in critical zones of the rotator cuff tendon is responsible for the degeneration of the tendon over time. (4,24) However, some evidence points to only the articular side of the tendon having hypovascularity. (4,24) To make matters more confusing degenerative tendons create more vessels within their matrix. Any potential positive of having more vessels for increased blood supply seems to be outweighed by the vessels crowding out vital collagen needed for tendon integrity. (24) As with aging the microvascular supply of our rotator cuff isn't something that we have much control over.
Side Note: It would make sense that the articular side of the tendon is prone to hypovascularity given the majority of rotator cuff tears occur there. (25)
3: Alterations in Tendon Matrix through Mechanical Overload and Overuse
If the demands placed on the tendon cells exceeds the ability of the tendon to repair and recover from that stress it leads to damage to the tendon over time. (4,24) This whole process is the same as described previously in the tendon continuum model.
Here are some potential mechanical overload scenarios:
- Introducing a powerlifting, strength training or olympic weightlifting program too quickly (Not being prepared for a given program and jumping straight into it) (26,27,28,29)
- Being a novice trainee (<6 months to 1 year training experience) (30,31)
- Lack of consistency with training (29,33)
- Excessive training volumes (eg: too much training via sets, reps, frequency, etc.) (26,27,28)
- Excessive training loads (using more weight then your shoulder can handle)
- Spikes in training volumes (eg: A sudden spike in training volume) (26,27,28)
What is excellent about this intrinsic factor is that we have total control over the amount of loading and recovery that we dose our tendons with over the course of time. What is the best dose of exercise is for the rotator cuff? That's the million dollar question.
4: Trauma
Any trauma to the rotator cuff tendons can also elicit the same process of degeneration as described previously in the tendon continuum model. (4,24)
Extrinsic Factors
Extrinsic factors were long thought to be the primary drivers of rotator cuff pathology for years. This thought process was responsible for the term "Subacromial Impingement Syndrome" or generic shoulder impingement.
The theory is all based around the subacromial space. The subacromial space sits between the acromion and the humeral head. More specifically the subacromial space refers to the structures that live under the "coracoacromial arch" or simply the structures that are below the acromion, the coracoid and the ligament that attaches those two structures.
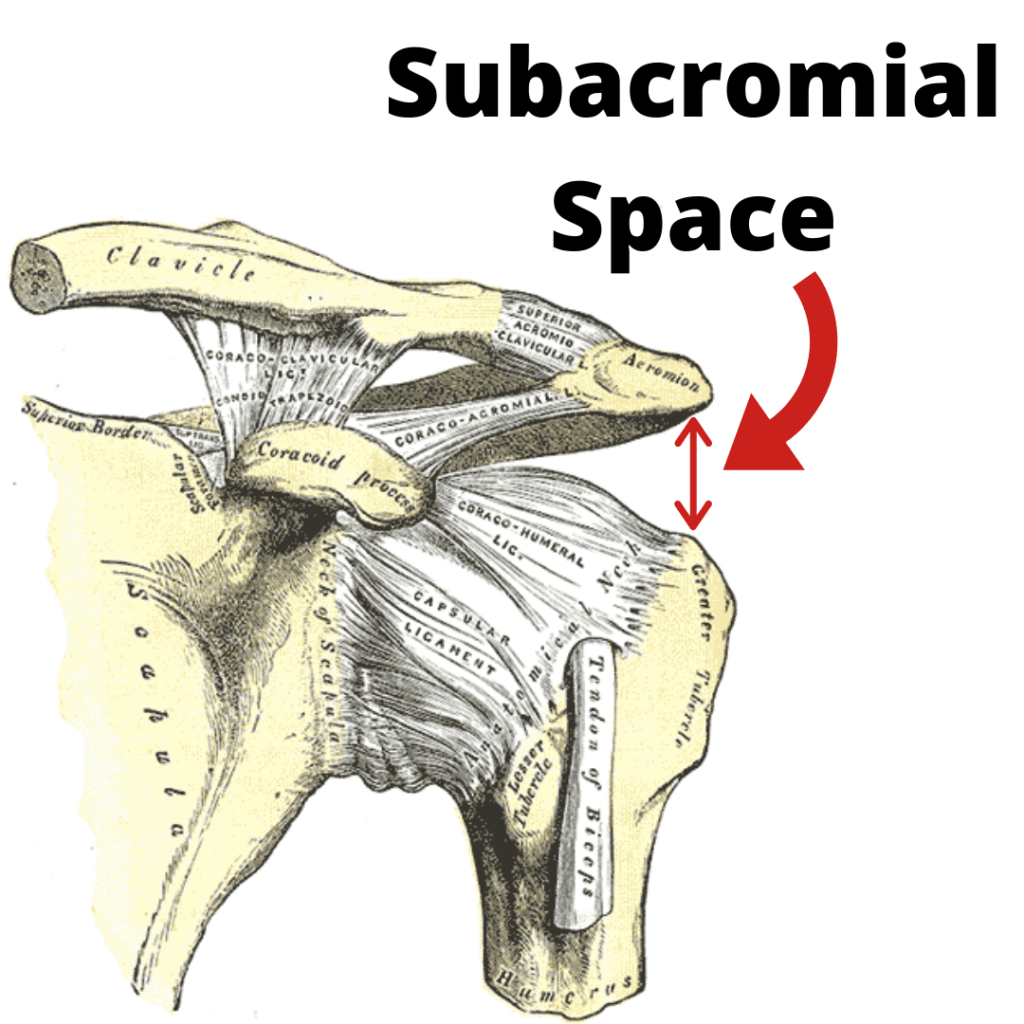
There are a few very important structures that sit in this space:
- Biceps Tendon
- Subacromial Bursa
- Supraspinatus Tendon
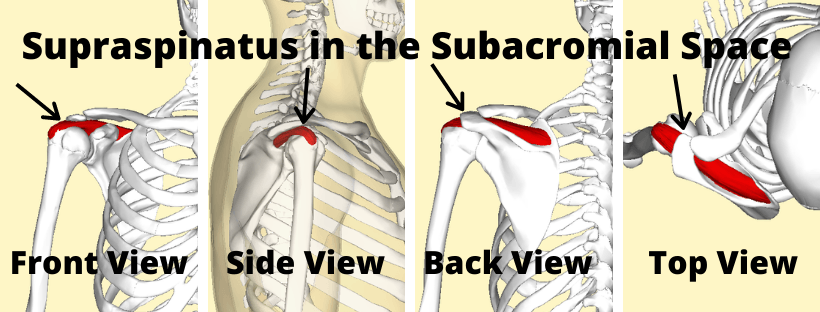
The idea is that these structures can be compressed or "impinged" when this space gets smaller. If there is excessive compression of these structures then over the course of time damage can occur and pain will result. If impingement was the primary culprit for rotator cuff tears then you'd expect most tears to occur on the bursal side of the tendon (right below the acromion). However, most tears actually occur on the articular side of the joint (right above the humerus). This is one of the main reasons we're starting to believe that intrinsic factors are more commonly the cause of rotator cuff tears and not extrinsic factors (subacromial impingement). (25)
With that being said, extrinsic factors do play a role in rotator cuff tears and bursal sided tears do exist so these variables can not be ignored. In some cases they may be the primary driver of cuff disease. (4, 24) Extrinsic variables include anatomical factors, biomechanical factors or both. (24) First we'll discuss anatomical factors.
1: Acromial Shape
Acromions come in all different shapes and sizes. Certain shapes also provide more or less space for the occupants of the subacromial space. Bigliani et al. were the first to describe 3 distinct types of acromions.
- Type 1 - flat
- Type 2 - curved
- Type 3 - hooked
Whether or not we're either born with these different acromion shapes or we acquire them over the course of time remains a controversial topic as well with mixed evidence on both sides (24)
2: Acromial Angle / Slope
As the slope of the acromion gets flatter towards horizontal, the subacromial space decreases. We have research to show that a more horizontal acromion is associated with subacromial impingement, degenerative changes of the cuff, subacromial spur formation and more loss of function in patients with tendinopathy. (24)
3: Arthritic and boney changes to the acromion, AC joint or coracoacromial ligament
With age arthritic changes to the AC joint occur. Among those changes are boney spurs (osteophytes) at the distal clavicle and acromion which can reduce the subacromial space. Spurs at the distal clavicle correlate with rotator cuff pathology. (24) Also keep in mind the correlation between arthritic changes and cuff pathology could be largely attributed to the patient's age and not necessarily due to a decreased subacromial space.
4: Abnormal Humeral Kinematics
The next few sections will talk about biomechanical reasons for extrinsic impingement.
The glenohumeral joint is a very mobile structure and a large majority of it's mobility is attributable to it's boney shape. It's a ball and socket joint and the socket is shallow enough to allow large ranges of motion. It is often described more like a golf ball on a tee as opposed to a ball and socket.
 Source: Attribution: Santeri Viinamäki / CC BY-SA (License)
Source: Attribution: Santeri Viinamäki / CC BY-SA (License)Given that the boney structure allows so much mobility, it doesn't provide much stability. For this reason the shoulder has a strong capsule or series of ligaments that surrounds the shoulder joint to provide additional stability. On top of that it has the rotator cuff to surround the joint and help keep the humeral head centered into the glenoid with movement.
When the deltoid fires to bring your arm overhead it also imposes a strong superior pull of the humerus. It's the job of the supraspinatus to pull the humeral head tight back into the glenoid.
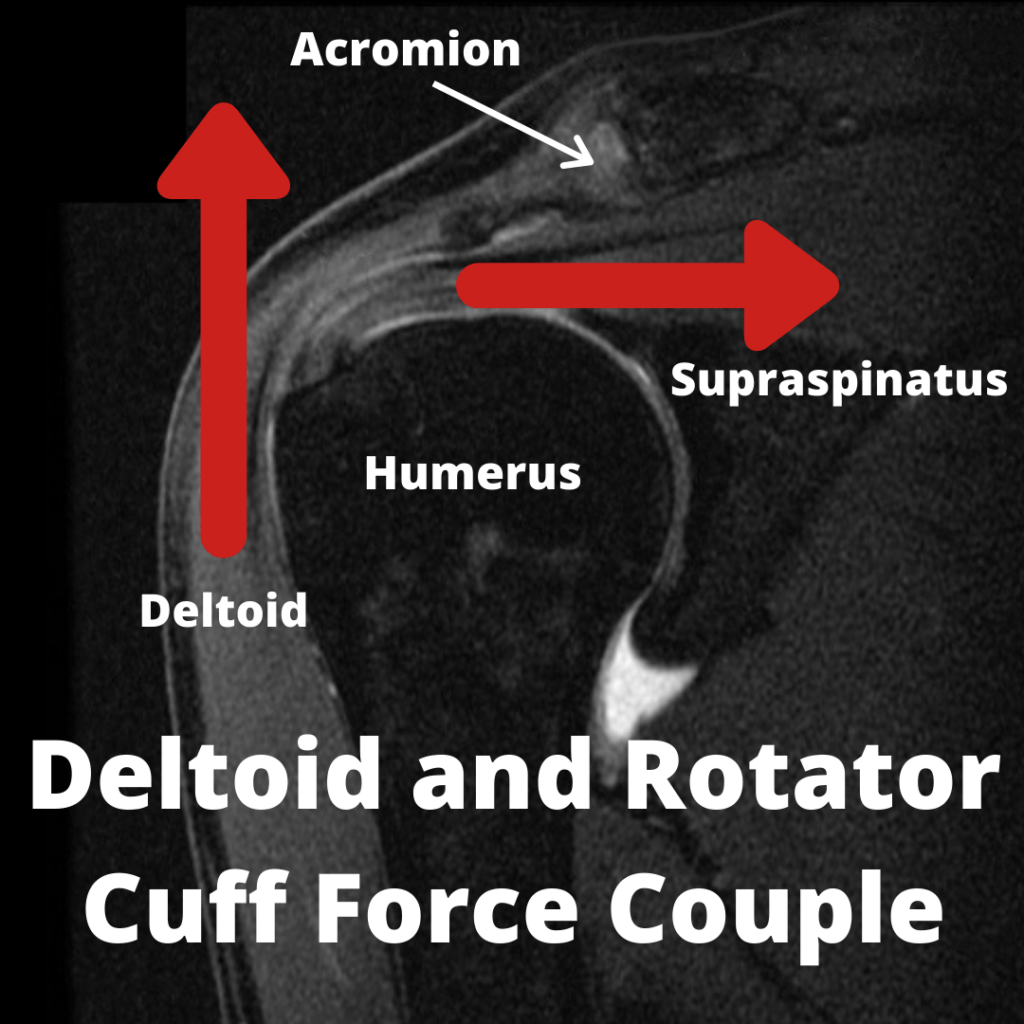 Image Source, Attribution: RSatUSZ / CC BY-SA (https://creativecommons.org/licenses/by-sa/4.0) - edited by Fitness Pain Free LLC
Image Source, Attribution: RSatUSZ / CC BY-SA (https://creativecommons.org/licenses/by-sa/4.0) - edited by Fitness Pain Free LLCThe same goes for the rest of the rotator cuff. As we bring the arm overhead the infraspinatus, teres minor and subscapularis all help to pull the humeral head into the glenoid. They also help to counter the superior translation of the humeral head by providing an inferior counterforce.
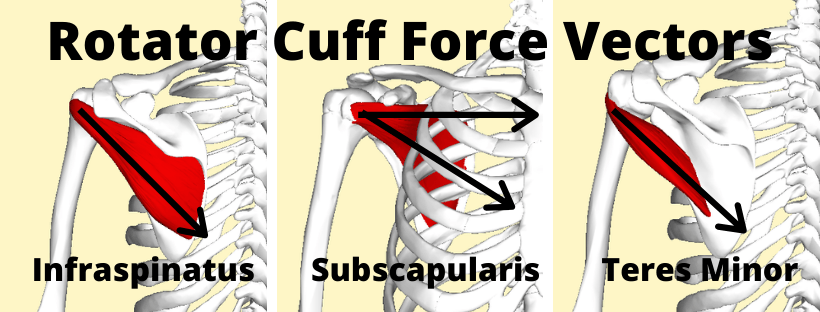 Image Source, License, Attribution: BodyParts3D/Anatomography – Edited by Fitness Pain Free LLC
Image Source, License, Attribution: BodyParts3D/Anatomography – Edited by Fitness Pain Free LLCSeveral biomechanical studies of the rotator cuff have shown that decreased rotator cuff forces (particularly the infraspinatus) results in superior humeral head motion. (24, 34)
Side Note: This evidence is mixed. One study in healthy people showed that induced paralysis of the supraspinatus and infraspinatus resulted in no effect on humeral head migration. (39)
If the rotator cuff is not doing it's job properly the humeral head can move from it's normal centered position. If the cuff specifically does not resist superior or upward motion of the humerus, the subacromial space will decrease and compression on the subacromial contents will occur.
We have evidence to support this as well (although you'll find conflicting evidence on this also). In folks with rotator cuff tendinopathy they presented with 1.0–1.5 mm greater superior translation as well as 3 mm anterior translation when raising their arms overhead when compared to a group without any pain or tendinopathy. (24) There is also evidence that pain alone can affect normal glenohumeral kinematics in shoulders with a structurally intact rotator cuff. (37)
We also have some evidence to show that patients with full thickness symptomatic cuff tears have reduced subacromial space and this space is increased after rotator cuff repair. (38) A significant loss of subacromial space prior to cuff repair surgery also correlates with poor prognosis after repair. (38) Rotator cuff tear size also correlates strongly with humeral head superior migration. (37)
So there is something about subacromial space and rotator cuff pathology.
Whether or not the superior translation occurs due to rotator cuff pathology or the superior translation leads to rotator cuff pathology is still up for debate.
My personal opinion is that they probably both effect one another. The superior translation can occur due to pain and rotator cuff pathology and the superior translation can also probably worsen the rotator cuff pathology / pain.
Side Note: It makes sense that a painful supraspinatus or infraspinatus would lead to superior migration of the shoulder. If pain inhibits the proper functioning of these muscles then the deltoid is free to move the humeral head superiorly with shoulder abduction without proper humeral head depression that normally occurs with a fully functional supraspinatus and infraspinatus.
5: Abnormal Scapular Kinematics
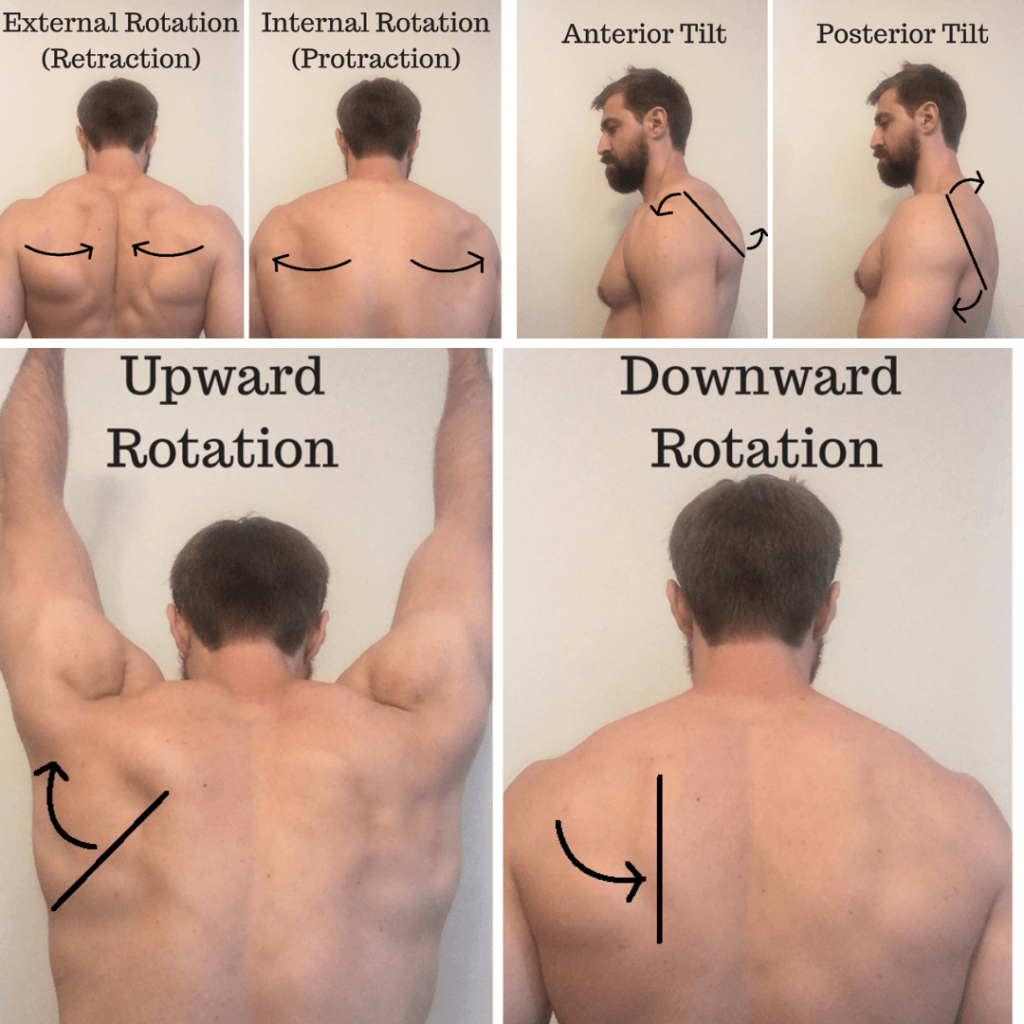
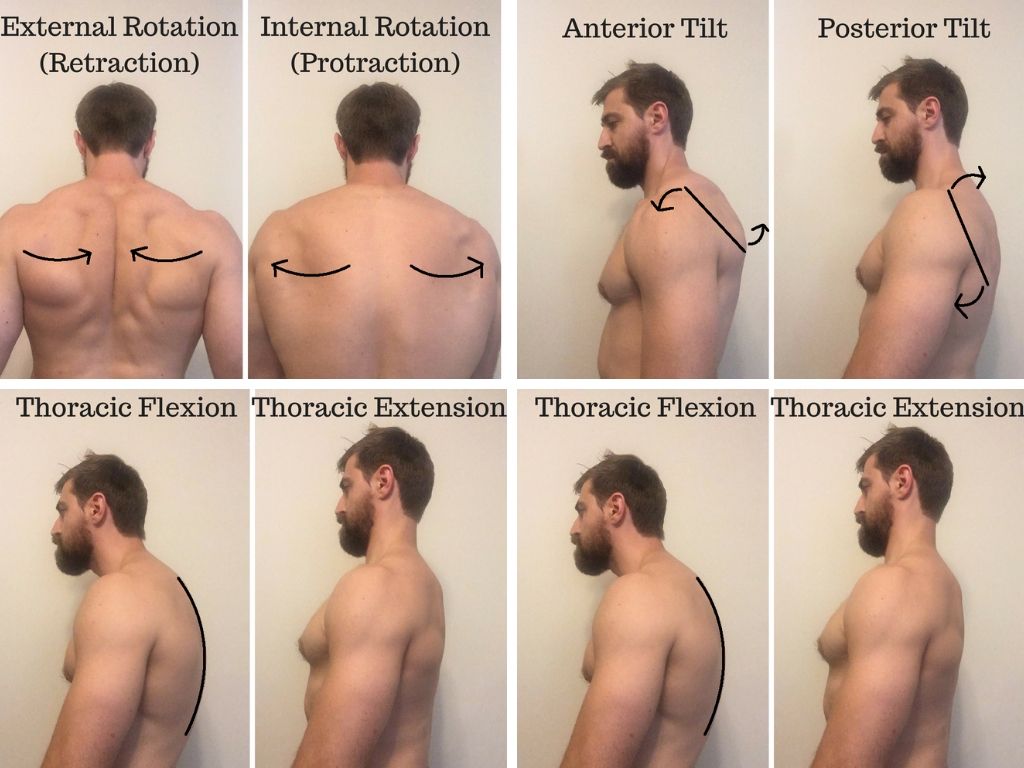
The idea behind abnormal scapular mechanics is pretty similar to altered glenohumeral mechanics. Basically, certain scapular positions can decrease the subacromial space and increase compression on the rotator cuff. These motions are:
- Scapular anterior tilt
- Scapular downward rotation
- Scapular internal rotation
As we bring our shoulder overhead if the scapular does not externally rotate, posteriorly tilt and upwardly rotate we decrease the subacromial space and compressive forces on the cuff are increased.
We have research to show that in comparison to normal people, folks with rotator cuff tendinopathy tend to present with reduced scapular posterior tilt, reduced scapular upward rotation and increased internal rotation in comparison to healthy folks. (24) However, we have research that shows the exact opposite in people with rotator cuff tendinopathy as well. Therefore it's not really fair to say that people with cuff tendinopathy and pain move in any specific way...
Side Note: It does make sense that having a painful cuff tendon that doesn't like to be compressed would drive increased scapular upward rotation, external rotation and posterior tilting to help increase space for the cuff.
I've provided some videos to help show you how movement from the shoulder blade helps free up space for the rotator cuff to breathe.
Scapular External Rotation (Retraction)
It is theorized that if we have weakness or altered firing of the scapular retractors (rhomboids / mid-trap) this may lead to scapular internal rotation and decreased subacromial space. (40) Scapular external rotation is also driven by thoracic extension whereas scapular internal rotation is driven by thoracic flexion.
Scapular Posterior Tilting
Having a tight pec minor can lead to scapular anterior tilting. Studies in people with a tight pec minor have shown decreased scapular posterior tilting at end range overhead reaching. (24)
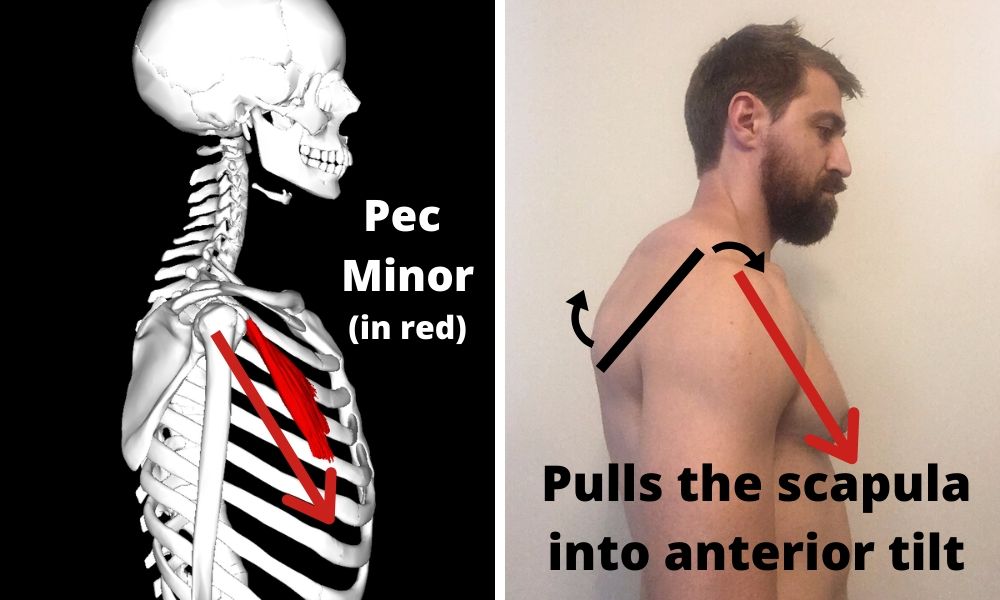
Weakness or altered muscle firing of the lower trapezius and serratus anterior is also thought to drive this problem. (8) Lastly, just as with scapular retraction, thoracic flexion also drives scapular anterior tilt.
Scapular Upward Rotation
Just as with compression of the rotator cuff due to abnormal glenohumeral mechanics, compression of the cuff due to a lack of upward rotation is thought to be caused by altered scapular force coupling of muscles:
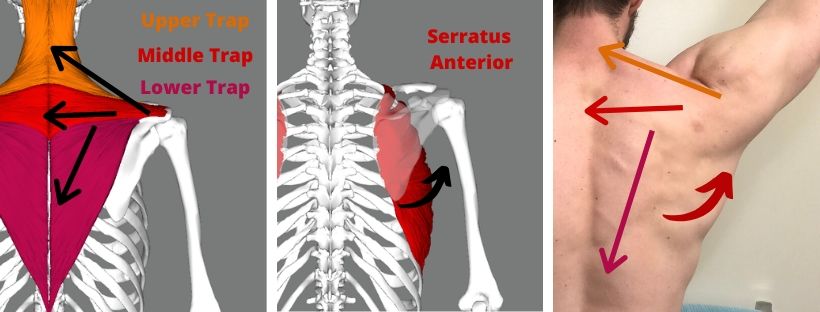
The trapezius and serratus anterior must all work together in synergy to allow for proper motion overhead. A lack of lower trapezius and serratus anterior activation and strength could limit upward rotation and create impingement issues. (8) Several studies have shown that those with rotator cuff tendinopathy have altered scapular muscle activity. (24) On top of that we have some research to show that people with cuff tendinopathy also have decreased muscle performance of the serratus anterior and lower trapezius when it comes to force output, muscle balance / ratios (upper vs. lower trap), EMG activity and delayed firing onset. (24)
This altered motion of the shoulder is often referred to as "scapular dyskinesis". Discussing dyskinesis thoroughly would be a long topic and is best discussed another day. I did want to touch on it a bit since it does have some implications for rotator cuff pathology.
Dyskinesis is actually quite a common finding in asymptmatic overhead athletes. (41) However, a study in 2018 in BJSM showed a 43% increased risk of shoulder pain in athletes who displayed dyskinesis. (41) Also, having dyskinesis is associated with poorer outcomes in those with shoulder pain. (41)
Unfortunately rehabilitation programs that focus on improving dyskinesia when compared to generic shoulder strengthening show better improvements in the dyskinesis group in the short term but no difference in the long term. (42) Even more disappointing, in the same study attempts to improve dyskinesia did not improve scapular positioning despite pain decreasing and function improving. (42)
Side Note: This may mean that we don't need to address the dyskinesia to have long term improvements in pain. It also may mean we need better treatments to correct dyskinesia if it truly is a player in the creation of rotator cuff pathology.
While we do have evidence that scapular mechanics can be altered in folks with rotator cuff tendinopathy, it's important to remember that this evidence is mixed. (24) The influence on scapular movement, subacromial compression and rotator cuff pathology is still speculative. (24) I will say that when I'm working with patient's I'll still work on normalizing their dyskinesia if I find it. I'm just not certain if it's going to make a difference beyond just applying a strength program.
6: Posture
Thoracic spine flexion is associated with scapular anterior tilt which has been shown to decrease the subacromial space as discussed previously. (24) This is also a hotly contested topic and you'll find research on both sides of the fence on whether or not posture relates to rotator cuff problems and pain. I personally don't want to open that bag of worms but suffice to say it can probably be a player in the pain process and it's something I'll address with my athletes as it certainly will impact the ability to perform overhead lifting well. (jerks, snatch, pull-ups)

What is the Clinical Presentation of Rotator Cuff Tears and Tendinopathy?
Rotator cuff injuries all present a bit differently from person to person but here are some of the hallmark signs you may find in these folks:
- Reduced shoulder function (4) (difficulty taking on and off shirts, reaching behind the back, putting on a jacket, reaching in the backseat of a car, overhead reaching)
- Scapular dyskinesis, pain, and stiffness. (4)
- Night pain while lying on the shoulder or sleeping with the arm overhead (4)
- Painful arc (4)
- Weak external rotators and supraspinatus (4)
- Positive special tests meant to provoke symptoms (Hawkin's Kennedy, Neer's) (4)
- Pain radiating to the lateral mid‐humerus or anterolateral acromion (4)
Clinical Reasoning for Strength and Fitness Athletes With Rotator Cuff Irritation
Now, your average person with shoulder pain isn't necessarily going to present like the strength or fitness athlete. Often times the athlete is going to be much less symptomatic then a 60 year old with a full thickness rotator cuff tear.
What I tend to see clinically in my cuff pain patients is pain during pressing exercises and at end ranges of motion (Like the catch of a snatch or back swing of a kip). I have a few theories as to why this may be. Keep in mind these are my own educated guesses, not established research.
Why Pressing is Generally More Painful Then Pulling and Rowing
Well, we have some pretty interesting studies that show which parts of the rotator cuff are most active during pressing exercises vs. pulling exercises. In general, pressing exercises are going to recruit more of the top (supraspinatus) and back (infraspinatus) portions of the rotator cuff. (21) On the flip side of the coin, rowing (glenohumeral extension) exercises preferentially recruit the front of the rotator cuff (subscapularis). (21)
The current theory as to why this happens is because the main job of the rotator cuff is to provide dynamic stability of the joint and keep the humerus centered in the glenoid during exercise.
Here's an example. When we bench press the deltoids and the pectorals provide a strong anterior pull to the humerus. This motion must be countered by the rotator cuff muscles on the back side of the joint:
The same thing goes for rowing / pulling movements:
You can use this logic to help figure out which movements may be provocative in the gym as well. If I perform resisted external rotation I know I'm recruiting the posterior cuff. If this is painful I may figure the infraspinatus is involved (keep in mind the suraspinatus is also active during resisted ER as well). I know the infraspinatus is heavily involved when performing both overhead pressing and horizontal pressing so I can also assume there is a chance that these motions might feel pretty poor when loaded in the gym.
Side Note: I'll ask a lot of questions about which movements are painful and not just assume based on my own clinical tests. We'll also perform a lot of trial and error in the gym and on the athlete's own to find the common culprits.
On top of this the supraspinatus takes more compressive stress through it's painful arc of motion. (22) We think this is the reason why rotator cuff patients have pain through a mid range of overhead motion. Also, this compression and tensile loading of the supraspinatus is only amplified by load. Some strength athletes may not have any shoulder pain during a normal painful arc but this arc shows up during heavier overhead press.
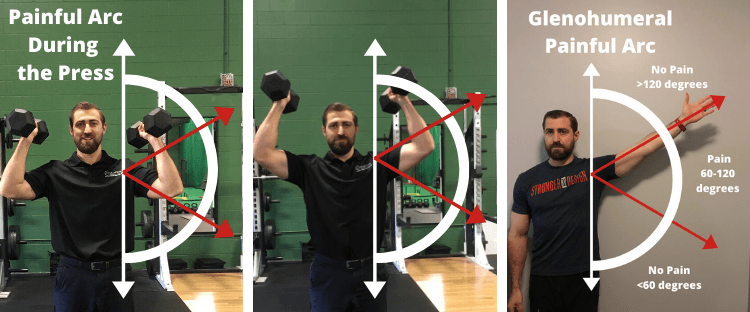
Side Note: More recent research into painful arc has shown most compression of the supraspinatus tendon insertion actually occurring at lower degrees of arm abduction (0-60 degrees) (22)
The other concept that may lend itself to more pain during pressing exercises is what happens to the subacromial space during press exercises. During the overhead press the deltoid muscle is very active as a prime mover during the movement. The deltoid not only helps bring the arm overhead but it also applies a strong superior pull to the humerus.
This superior pull has to be countered by the rest of the rotator cuff to keep the humerus centered into the glenoid during overhead motions. We know that the simple act of bringing the arm overhead reduces the subacromial space and compresses the cuff. If we have an irritated rotator cuff on our hands then we may get some pain when going overhead.
Pulling exercises like a dumbbell row or lat pull down actually have the opposite effect on the subacromial space. When we perform a row or resisted extension the lats impose a strong pull inferiorly and posteriorly to the humerus.
This actually increases the subacromial space. We have some proof of concept research to show that a resisted isometric into extension of the shoulder held at 90 degrees of shoulder flexion increases subacromial space. (43) Less compression could equal less pain and subsequently a lot of folks with shoulder pain who tolerate pulling well but not pressing.
Why End Ranges Are More Painful then Mid Ranges During Exercise
The next concept to discuss are end ranges. End ranges of motion like full overhead flexion can be irritating to the cuff. I often see patients who can't tolerate the catch of the snatch or backswing of a kipping motion. The same goes for full range dips. Now, I don't have a great answer for this but I have some theories...
1: End ranges overhead can increase compressive forces on the rotator cuff
Well for one, we have orthopedic tests that purposefully take our shoulder to end ranges of motion to assess whether or not the rotator cuff tendons are irritated. 1 classic test is the Neer's Test. This test was designed to take the acromion into contact with the cuff tendons and if irritated, elicit pain.
Several gym movements mimic this position. The catch of the snatch and the backswing of ring movements are two good examples.

The back swing of a kip and catch of the snatch requires most of, if not end range flexion. If we combine some of this flexion with internal rotation we're creating a loaded Neer's test position.
Any time we bring the arm overhead we're bringing the insertion of the rotator cuff closer to the acromion. Check out the images below to see what I'm talking about.
Side Note: Research over the course of time has been very mixed in terms of whether or not the Neer's test even compresses the cuff tendons. You can readily find articles that even show the Neer's test position compresses the cuff LESS then a mid-range of shoulder abduction (23)
Another possible form of compression of the rotator cuff comes from compression against the glenoid. Research on the Neer's test is mixed in terms of compression from the acromion but the same position (flexion and internal rotation) does consistently show contact between the rotator cuff tendons and the glenoid. This goes for a variety of end range positions:
- Flexion (60, 64)
- Abduction and external rotation (classic internal impingement present in overhead athletes like pitchers)
- Flexion and Internal rotation (Neer's position) (60,61,63,64)
This form of compression is actually well documented in baseball pitchers as the major cause of injury in the rotator cuff (infra). (60,64) One study (61) actually demonstrated that the position where the Neer's test was symptomatic correlated with where the cuff makes contact with the glenoid in flexion while the patient was under anesthesia later for shoulder surgery.
Given that this type of compression would create articular sided rotator cuff tears it stands to reason that this may be the major form of compression causing cuff pathology and not from the acromion.
2: End ranges of motion create more humeral translation within the joint
We've all heard of the roll and glide of a joint. If you haven't the concept is fairly simple. In a ball and socket joint like the shoulder we'll have the humeral head spin within the joint as the arm moves and we'll also have the humeral head translate with it (glide).
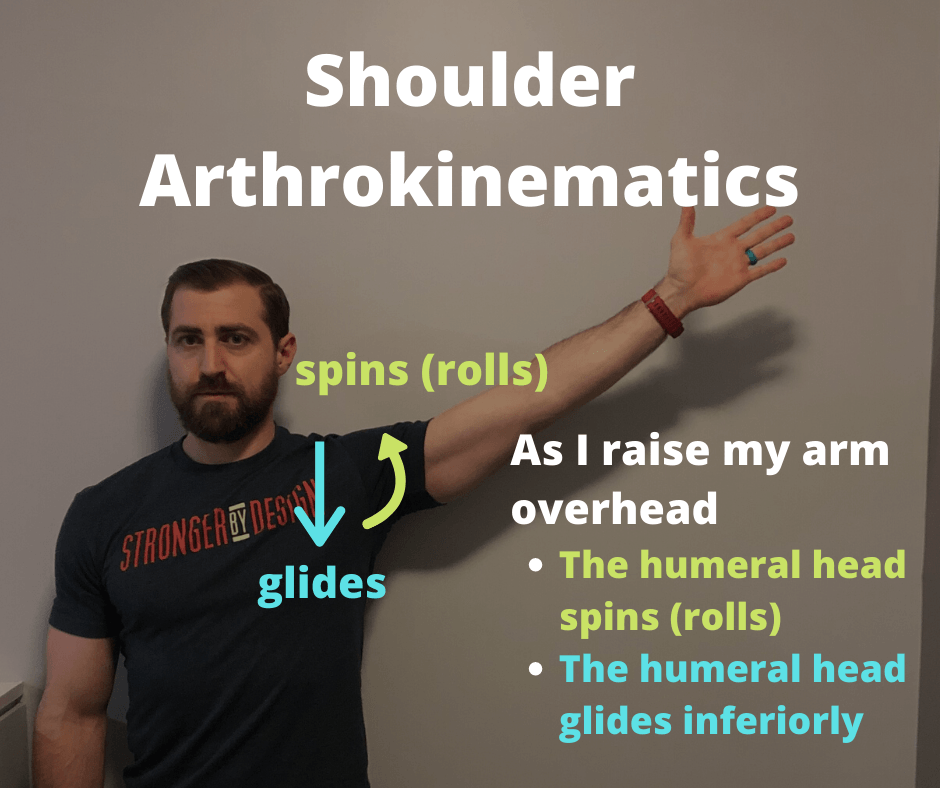
Which direction the humeral head glides depends on which way you move your shoulder joint.
- Extension / horizontal abduction / external rotation = Anterior
- Flexion = Inferior
- Internal rotation / horizontal adduction = Posterior
The shoulder joint moves in the opposite direction when we extend the shoulder as in a dip:
As discussed previously, the rotator cuff's job is to control motion within the glenohumeral joint. Basically it's attempting to keep the humerus centered in the glenoid as we move our arms around and train in the gym. Think about the example earlier about how the posterior cuff has to fire to counter the anterior translation that comes from the force of the pecs contracting.
As we approach end ranges of motion, we have more and more translation occurring within the joint. This means that the cuff's job gets a little more challenging at end ranges as well because it has to work hard to counter these increased forces.
2: End ranges of motion create weaker length / tension relationships
Muscles are strongest when they are asked to produce force in their mid range of motion. In other words muscles are at their weakest when they are either fully stretched or fully shortened.
When you take a joint to it's end range of motion you've generally shortened the muscles on one side of the joint and stretched the muscles on the other side of the joint.
Think for example the bench press. In the bottom of the bench press the shoulder is sitting in extension and horizontal abduction. The prime movers for the shoulder in this situation are going to be the anterior deltoid and the pecs. Both of these muscles are fully stretched in this position and thus weaker then if we were in a mid range of motion.
On the back side of the joint you've got the lats which are now maximally shortened and thus weaker. Now the cuff has to work even harder to make up for the lack of stability coming from musculature that is maximally shortened or lengthened.
Not to mention the cuff itself is probably undergoing a fair bit of shortening and stretching at end ranges of motion decreasing it's ability to control motion within the glenohumeral joint as we get into end ranges of motion.
Why Load and Volume is Even More Important for Strength and Fitness Athletes
Earlier in the article we discussed how overload to the tendon could be one of the most important factors in the progression of healthy tendons to pathological tendons to tears. We also discussed the potential of a lack of stress to a tendon creating pathology as well.
We have a plethora of research coming out showing just how closely training loads correlate with risk of injury. (26, 27, 28) More notably, when we expose our athletes to training stresses they are not adequately prepared for their risk of injury increases. (26, 27, 28)
Load and volume in the gym can be calculated in a variety of ways:
- Weight on the bar (intensity / load)
- Perceived effort during sets and sessions
- Duration of training sessions (daily, weekly and monthly)
- Total reps per session / week
- Total sets per session / week
- Frequency of exercise prescription (how many days / week did you bench press)
As fitness and rehab professionals we have a tremendous ability to influence these variables for our athletes and potentially have a big impact on whether or not injury occurs.
With this being said, we are often more concerned with other potential reasons for injury without addressing load and volume. Undoubtedly the training programs written for these athletes will be a major decider of whether or not an athlete adapts and improves or ends up getting injured.
The same goes for injured athletes. Our ability to dose exercise may be one of the most important abilities to allow our athletes to recover and get back to training.
Keep in mind that these are all of my own theories based on what I see clinically, evidence based decision making, science and logic. They are not well established injury mechanisms, just my thoughts.
Rehabilitation and Expectations
To start, this article is not designed to talk about in depth rehabilitation strategies in folks with shoulder pain. I've done this in another article. Click HERE if you'd like to see my complete guide to rehabilitating shoulder pain.
The majority of rehab studies generally show positive outcome for folks with both rotator cuff tendinopathy and tears. (47) After undergoing physical therapy most patients report improvements in both pain and function. The majority of rehab programs last somewhere between 6 and 12 weeks and improvements are usually seen by the 12 week mark. (47) (Always keep in mind that some people improve faster and others slower.)
Just how much patients improve varies from study to study but keep in mind that most people made IMPROVEMENT over the time period, not a complete resolution of symptoms. (49) This is important to keep in mind when educating your athletes about expectations with rehab. You may find your athletes expecting to be 100% after therapy and that may not be reasonable. With that being said, there are certain indicators that will predict more improvement with rehab.
What Factors Increase Likelihood of Success With Physical Therapy?
Prognostic factors for success with physical therapy:
- Good abduction strength
- External rotation ROM >52 degrees
- Negative Impingement Signs
- Little to no atrophy of the supraspinatus
- Preserved intramuscular tendon of supraspinatus
What factors decrease the likelihood of success with physical therapy
- Restricted range of motion
- Tears extending from the supraspinatus to the infraspinatus
- Full thickness tears >1cm combined with symptoms >1 year
- Functional impairments and weakness
- Emotional Distress (51)
Basically, exercise therapy seems to be helpful for all types of rotator cuff pathology. This goes for tendinopathy, all of the way down to massive full thickness tears. (52) With that being said, a conservative approach is not always the best choice for our cuff patients...
Who are the Best Surgical Candidates?
As stated earlier, not everyone is going to need surgery. For many people surgery is not the best option. However, in some people surgery may be the best option. Surgical repair of the rotator cuff is one of the most common orthopedic procedures performed and accounts for approximately 75,000 operations each year in the USA alone (58)
There are several factors to consider when deciding if someone's best course of action is surgery:
- Symptoms (pain / disability)
- Full thickness vs. partial thickness
- Size of tear
- Whether the injury is acute vs. chronic vs. both
First off, we know there are a ton of asymptomatic tears out there. Currently we don't believe it's a good idea to start repairing cuff tendons unless they actually hurt. Second of all, we know that full thickness and larger partial thickness tears tend to progress more quickly then smaller tears. For this reason having a larger or full thickness tear bumps up the decision making process in favor of surgical repair. (especially if you're on the younger side of life) Lastly, acute traumatic tears are more often repaired earlier then chronic tears. We'll discuss this more a bit later.
The decision of undergoing surgery must be tailored to the person and their activity level as well. The traditional thought is that a higher level athlete will need a fully functioning rotator cuff to perform at a high level of function where as a person who doesn't need their shoulder for high level functioning might not need the surgery.
Tashjian et al. (48) presented a decision making algorhythm to help decide who needed surgery and who doesn't. It's a pretty useful tool. The authors lumped people into 3 different groups to help decide the best course of action for folks with rotator cuff tears.
Group one: Initial conservative treatment: (48)
- Chronic, full thickness tears, age >60 years old
- Anyone with a large or massive RC tear
- Irreparable tears (based on tear size, retraction, muscle quality and migration)
Folks in this group are recommended to attempt physical therapy first before trying surgery. What are the reasons for this? For one, age matters:
Only 43% of patients over the age of 65 treated with arthroscopic rotator cuff repair of a full-thickness supraspinatus tear had evidence of healing at 18 months postoperatively compared with 86% of patients under 65. (49)
In other words the surgical repair of cuff tendons fails (just doesn't heal) much more frequently (twice as often) in folks over the age of 65 as compared to those under the age of 65. Since cuff repair has such a high chance of failing then physical therapy is an easy first option. If therapy is not successful surgery can always be considered after. (49) Those who fail conservative treatment are often the most obvious choice for surgical repair. (58)
Group two: Early Surgical Repair: (48)
- All acute tears >1 cm
- All chronic full thickness tears >1cm and patient age <60 years old
The rationale in this group is that patients with acute tears or chronic full thickness tears under the age of 60 run the risk of irreversible damage in the future if the tendon is not repaired. Another reason that the treatment of choice for traumatic rotator cuff tears is surgical repair is simply because the outcomes are good. These rotator cuff repairs tend to really reduce pain and people can return to their prior level of activity. Also surgical repair of traumatic tendon injuries in younger folks have been shown to be more successful then surgery in atraumatic tendon tears in older folks. (49)
If a tendon is left torn and not surgically repaired it may lose elasticity, enlarge and make the possibility of a future repair more challenging and potentially worsen outcomes. For this reason it may be best to do the repair early and prevent future wear and tear.
Side Note: Bjornsson and colleagues challeneged this thought process showing that no differences existed when comparing tendon healing, pain shoulder motion or functional outcomes in a group having their rotator cuff repaired within 3 weeks of the initial injury vs. 3 months after the initial injury. (50) I'd like to see if this same result would extend out to 6 months to a year or multiple years. (I'd figure not...)
Despite atraumatic chronic cuff tears doing well with physical therapy in older patients we still don't know how to best manage atraumatic cuff tears in younger and more active folks. Given the large amount of research showing the rates of cuff tear progression it may be wise to surgically repair these folks sooner rather then later. (49)
Group 3: Prolonged Conservative Treatment: (48)
- Tendinopathy
- Partial Thickness Repairs
- Small <1cm full thickness tears
In folks with just tendinopathy, partial thickness or small full thickness tears prolonged conservative treatment is recommended. This is because these issues tend to have a slower rate of progression then larger tears. This group also tends to do really well with conservative treatment like physical therapy. (49)
What's also nice is that pain is usually correlated with tear progression and can serve as a warning sign in these folks if something is worsening. (49)
Lastly, as described earlier in the article shoulder activity and overuse can be attributed to worsening rotator cuff issues. Keep in mind that this research is mixed in the general population (44) but in the athletic population it may be more relevant.
How Many People Will Go On To Require Surgery After Failing Conservative Treatment?
In group 1 we discussed that these folks should trial physical therapy before moving on to attempt surgery. Well, just how many people will end up needing surgery? Check out the study below for some answers:
The Moon Shoulder Group (44)
- Atraumatic full thickness rotator cuff tears: 381 patients (mean age 62 years, range 31-90) followed for a minimum of two years
- 6-12 weeks of physical therapy (Cuff strengthening and mobility)
- Improvements in functional outcomes were shown (patient reported)
- 9% chose to have rotator cuff repair surgery (6 weeks into therapy).
- 6% chose to have rotator cuff repair surgery (12 weeks into therapy)
- In total, 26% of patients decided to have surgery by the two-year follow-up.
- Patients most likely to undergo surgery in the 1st 12 weeks. Patients unlikely to undergo surgery if they make it beyond 12 weeks.
Side Note: Interestingly, the patients who decided to undergo surgery may have simply not waited long enough to see the benefits of therapy based on the current time frame required to see benefit from therapy. These patients may have "jumped the gun" too quickly for surgery.
Surgery vs. Physical Therapy
Sometimes it isn't completely clear who should have surgery and who shouldn't. We actually have a few studies out there to compare surgery with more conservative treatment to help us decide.
Kukkonen et al (45)
- 3 different methods for treating symptomatic - nontraumatic tears of the supraspinatus
- 167 patients aged >55
- Physical therapy vs. acromioplasty and physical therapy vs. rotator cuff repair, acromioplasty and physical therapy
- All groups reported improvements in pain and reported functional outcome
- No differences in groups reported at 1 year follow up
In this study there was actually no difference in outcome between all 3 groups. The authors noted that given this fact physical therapy treatment seems very worthy as a primary first treatment in these folks. Littlewood et al came to the same conclusion in their systematic review on rotator cuff tear treatment stating that exercise therapy is similar in it's ability to reduce pain and restore function in comparison to surgery. (47)
Side Note: Studies like this bring up the need for placebo controlled trials to see if surgery really is beneficial for patients. Currently we don't know if surgery for rotator cuff tears works as well as placebo (sham surgeries). However, we do have some trials currently underway trying to figure this out in acute traumatic tear populations. Also, shoulder surgery if often combined with physical therapy afterwards so we aren't always sure if the surgery fixed the issue or the exercise was the key.
Despite the surgical group improving as well as the physical therapy groups there is still a risk for tear progression over time in the physical therapy only patients. Continued and ongoing monitoring will be very important for these folks to make sure the tears are not progressing rapidly.
Moosmayer et al (46)
- Rotator cuff tears <3 cm in size
- Non-operative treatment (physical therapy) vs. Surgery
- Outcomes improves in both groups
- Outcomes better in surgery group at 12 months
- Only 17% of therapy group failed treatment and elected for surgery
- 37% of cuffs treated with physical therapy went on to increase cuff tear size >5 cm at 5 year follow up
This next study actually showed that the surgical group ended up having better outcomes then physical therapy. On top of that they also followed up patients who did not receive surgery and 37% of those folks had their tear increase to >5 cm in the next 5 years. This may give more credibility to the idea of repairing the cuff to prevent long term damage.
Rotator Cuff Surgery Outcomes
Rotator cuff surgery generally goes pretty well with the majority of people reporting improvements in pain and function after surgery. (57, 58) A 2018 review article by Novoa‐Boldo et al. showed 90% of patients reported they were happy with their procedure 6 months following surgery. (58)
With that being said, some surgeries are going to go better then others. On top of that choosing the right candidates for surgery can also go a long way. We have some data to help us decide who's going to do well with surgery.
What Factors Worsen Surgical Outcomes After Cuff Repair? (54)
- Older age
- Larger tear size
- Worse muscle quality (atrophy and presence of fatty infiltrate)
- Greater muscle tendon retraction (tendon insertion pulling away from the humerus)
- Smoking
- Osteoporosis (low bone mineral density)
- Vitamin D deficiency
- Diabetes (altered blood sugar)
- Hypercholesterolemia
If you have someone with a big chunk of these factors, you may think twice prior to sending them off to have a cuff repair.
There is also always a chance the cuff will re-tear following surgical repair. Actually a surprisingly large chunk of rotator cuff repairs will tear again following surgery. Depending on the study and the population rotator cuff failures are seen in 20 to 94% of patients after rotator cuff repair.
Obviously the factors mentioned previously play a role in the rate of rotator cuff re-tears. For example the relative risk of re-tear increases 2.29 times with every 1 cm increase in tear size. (55)
Remarkably, it has been observed in patients whose repairs fail after surgery, that reported satisfaction levels and clinical outcome scores are similar to those with intact repairs. (49) What this means is that you can have a rotator cuff tear and get it repaired and have it feel and move better despite it being re-torn again. This also means that if people had a re-tear of their cuff they may not even know about it
However, in patients that had re-tears they were slightly more painful and had decreased strength in comparison to surgeries with an intact cuff still. (59) However, the majority of people did not have a clinically meaningful difference in function or pain whether or not the cuff re-tore or not. (59)
and.....
You've finally made it to the end!! I hope you enjoyed this guide to rotator cuff injuries. If you're interested in learning how I personally like to help these athletes get out of pain and back to training click HERE for another article I've written on the subject.
Writing this article has retracted my rotator cuff,
Dan Pope DPT, OCS, CSCS
References:
Mehrab, M., de Vos, R.-J., Kraan, G. A., & Mathijssen, N. M. C. (2017). Injury Incidence and Patterns Among Dutch CrossFit Athletes. Orthopaedic Journal of Sports Medicine
Ulrika Aasa et al. Injuries among weightlifters and powerlifters: a systematic review BJSM 2017
David Factor, Barry Dale CURRENT CONCEPTS OF ROTATOR CUFF TENDINOPATHY Int J Sports Phys Ther. 2014 Apr; 9(2): 274–288. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4004132/
Minagawa, H., Yamamoto, N., Abe, H., Fukuda, M., Seki, N., Kikuchi, K., … Itoi, E. (2013). Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. Journal of Orthopaedics, 10(1), 8–12 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3768248/
Lewis, J. S. (2009). Rotator cuff tendinopathy: a model for the continuum of pathology and related management. British Journal of Sports Medicine, 44(13), 918–923. https://www.ncbi.nlm.nih.gov/pubmed/19364757
Malliaris et. al. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations JOSPT https://www.jospt.org/doi/pdf/10.2519/jospt.2015.5987?code=jospt-site
Physio Edge 075 Tendinopathy, imaging and diagnosis with Dr Sean Docking https://www.clinicaledge.co/podcast/physio-edge-podcast/75
Andrew Carr, The Epidemiology, Pathology, and Treatment of Rotator Cuff Tears, Sports Medicine Congres shttps://youtu.be/eXZGRpa19DA
Muto, T., Inui, H., Ninomiya, H., Tanaka, H., & Nobuhara, K. (2017). Characteristics and Clinical Outcomes in Overhead Sports Athletes after Rotator Cuff Repair. Journal of Sports Medicine, 2017, 1–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5494057/
Pennock, A. T., Dwek, J., Levy, E., Stearns, P., Manning, J., Dennis, M. M., … Taylor, K. S. (2018). Shoulder MRI Abnormalities in Asymptomatic Little League Baseball Players. Orthopaedic Journal of Sports Medicine, 6(2), 232596711875682. https://journals.sagepub.com/doi/full/10.1177/2325967118756825
Summitt, R. J., Cotton, R. A., Kays, A. C., & Slaven, E. J. (2016). Shoulder Injuries in Individuals Who Participate in CrossFit Training. Sports Health: A Multidisciplinary Approach, 8(6), 541–546. https://www.ncbi.nlm.nih.gov/pubmed/27578854
Cook, J. L., & Purdam, C. R. (2008). Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. British Journal of Sports Medicine, 43(6), 409–416. https://www.ncbi.nlm.nih.gov/pubmed/18812414/
Kim, H. M., Dahiya, N., Teefey, S. A., Middleton, W. D., Stobbs, G., Steger-May, K., … Keener, J. D. (2010). Location and Initiation of Degenerative Rotator Cuff Tears. The Journal of Bone and Joint Surgery-American Volume, 92(5), 1088–1096. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2945926/
Jeong, J. Y., Min, S. K., Park, K. M., Park, Y. B., Han, K. J., & Yoo, J. C. (2018). Location of Rotator Cuff Tear Initiation: A Magnetic Resonance Imaging Study of 191 Shoulders. The American Journal of Sports Medicine, 46(3), 649–655. https://www.ncbi.nlm.nih.gov/pubmed/29314867
Kuzel, B. R., Grindel, S., Papandrea, R., & Ziegler, D. (2013). Fatty Infiltration and Rotator Cuff Atrophy. Journal of the American Academy of Orthopaedic Surgeons, 21(10), 613–623. https://www.ncbi.nlm.nih.gov/pubmed/24084435
Codding, J. L., & Keener, J. D. (2018). Natural History of Degenerative Rotator Cuff Tears. Current Reviews in Musculoskeletal Medicine, 11(1), 77–85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5825342/
Nathani, A., Smith, K., & Wang, T. (2018). Partial and Full-Thickness RCT: Modern Repair Techniques. Current Reviews in Musculoskeletal Medicine, 11(1), 113–121. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5825346/
Mall, N. A., Kim, H. M., Keener, J. D., Steger-May, K., Teefey, S. A., Middleton, W. D., … Yamaguchi, K. (2010). Symptomatic Progression of Asymptomatic Rotator Cuff Tears. The Journal of Bone and Joint Surgery-American Volume, 92(16), 2623–2633. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2970889/
Wattanaprakornkul, D., Halaki, M., Cathers, I., & Ginn, K. A. (2011). Direction-specific recruitment of rotator cuff muscles during bench press and row. Journal of Electromyography and Kinesiology, 21(6), 1041–1049. https://www.ncbi.nlm.nih.gov/pubmed/21978788
Lawrence, R. L., Schlangen, D. M., Schneider, K. A., Schoenecker, J., Senger, A. L., Starr, W. C., … Ludewig, P. M. (2017). Effect of glenohumeral elevation on subacromial supraspinatus compression risk during simulated reaching. Journal of Orthopaedic Research, 35(10), 2329–2337. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5503805/
Roberts, C. S., Davila, J. N., Hushek, S. G., Tillett, E. D., & Corrigan, T. M. (2002). Magnetic resonance imaging analysis of the subacromial space in the impingement sign positions. Journal of Shoulder and Elbow Surgery, 11(6), 595–599. https://www.ncbi.nlm.nih.gov/pubmed/12469085
Seitz, A. L., McClure, P. W., Finucane, S., Boardman, N. D., & Michener, L. A. (2011). Mechanisms of rotator cuff tendinopathy: Intrinsic, extrinsic, or both? Clinical Biomechanics, 26(1), 1–12. https://www.ncbi.nlm.nih.gov/pubmed/20846766/
Lewis, J. S., & Sandford, F. M. (2009). Rotator Cuff Tendinopathy: Is There a Role for Polyunsaturated Fatty Acids and Antioxidants? Journal of Hand Therapy
The Development and Application of an Injury Prediction Model for Noncontact, Soft-Tissue Injuries in Elite Collision Sport Athletes. (n.d.). Retrieved August 01, 2016, from https://www.researchgate.net/publication/46288877_The_Development_and_Application_of_an_Injury_Prediction_Model_for_Noncontact_Soft-Tissue_Injuries_in_Elite_Collision_Sport_Athletes
Relationship Between Training Load and Injury in Professional Rugby League https://www.researchgate.net/profile/Tim_Gabbett/publication/49775412_Relationship_between_training_load_and_injury_in_professional_rugby_league_players/links/551894590cf2d70ee27b41ad.pdf
Training and game loads and injury risk in elite Australian footballers. (n.d.). Retrieved from https://www.researchgate.net/profile/Brent_Rogalski/publication/234699103_Training_and_game_loads_and_injury_risk_in_elite_Australian_footballers/links/53dadd6b0cf2a19eee8b3f9f.pdf
The risk of injuries among CrossFit athletes: an Italian observational retrospective survey. Tafuri S1, Salatino G2, Napoletano P3, Monno A4, Notarnicola A
A 4-Year Analysis of the Incidence of Injuries Among CrossFit-Trained Participants Orthop J Sports Med. 2018 Oct; 6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6201188/
Injury Incidence and Patterns Among Dutch CrossFit Athletes Orthop J Sports Med. 2017 Dec; 5(12): 2325967117745263. Published online 2017 Dec 18. doi: 10.1177/2325967117745263 Mirwais Mehrab, BSc,*† Robert-Jan de Vos, MD, PhD,‡ Gerald A. Kraan, MD, PhD,† and Nina M.C. Mathijssen, PhD†
Injury Rate and Patterns Among CrossFit Athletes Orthop J Sports Med. 2014 Apr; 2(4): 2325967114531177. Benjamin M. Weisenthal, BA,* Christopher A. Beck, MA, PhD,† Michael D. Maloney, MD,‡ Kenneth E. DeHaven, MD,‡ and Brian D. Giordano, MD‡§
Musculoskeletal injuries in Portuguese CrossFit practitioners. J Sports Med Phys Fitness. 2019 Feb 5. [Epub ahead of print] Minghelli B1, Vicente P2.
Mura, N., O’Driscoll, S. W., Zobitz, M. E., Heers, G., Jenkyn, T. R., Chou, S.-M., … An, K.-N. (2003). The effect of infraspinatus disruption on glenohumeral torque and superior migration of the humeral head: A biomechanical study. Journal of Shoulder and Elbow Surgery, 12(2), 179–184. https://www.ncbi.nlm.nih.gov/pubmed/12700573/
Leong, H., Fu, S., He, X., Oh, J., Yamamoto, N., & Yung, S. (2019). Risk factors for rotator cuff tendinopathy: A systematic review and meta-analysis. Journal of Rehabilitation Medicine, 0. https://www.ncbi.nlm.nih.gov/pubmed/31489438
McMahon, P. J., Prasad, A., & Francis, K. A. (2014). What Is the Prevalence of Senior-athlete Rotator Cuff Injuries and Are They Associated With Pain and Dysfunction? Clinical Orthopaedics and Related Research®, 472(8), 2427–2432. https://www.ncbi.nlm.nih.gov/pubmed/24619795
Keener, J. D., Wei, A. S., Kim, H. M., Steger-May, K., & Yamaguchi, K. (2009). Proximal Humeral Migration in Shoulders with Symptomatic and Asymptomatic Rotator Cuff Tears. The Journal of Bone and Joint Surgery-American Volume, 91(6), 1405–1413. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2686133/
Pepe, M., Kocadal, O., Gunes, Z., Calisal, E., Aksahin, E., & Aktekin, C. N. (2018). Subacromial space volume in patients with rotator cuff tear: The effect of surgical repair. Acta Orthopaedica et Traumatologica Turcica. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6318497/
Werner et al., 2006Werner, C.M., Weishaupt, D., Blumenthal, S., Curt, A., Favre, P., and Gerber, C. Effect of experimental suprascapular nerve block on active glenohumeral translations in vivo. J. Orthop. Res. 2006; 24: 491–500
EXERCISE REHABILITATION IN THE NON-OPERATIVE MANAGEMENT OF ROTATOR CUFF TEARS: A REVIEW OF THE LITERATURE Peter Edwards, MSc,1 Jay Ebert, PhD,1 Brendan Joss, PhD,1 Gev Bhabra, FRCS,3 Tim Ackland, PhD,1 and Allan Wang, PhD, FRACS1,2,3 Int J Sports Phys Ther. 2016 Apr; 11(2): 279-301 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC48273718
Hickey D, Solvig V, Cavalheri V, et al Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis British Journal of Sports Medicine 2018;52:102-110. https://bjsm.bmj.com/content/52/2/102.long
Struyf, F., Nijs, J., Mollekens, S., Jeurissen, I., Truijen, S., Mottram, S., & Meeusen, R. (2012). Scapular-focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clinical Rheumatology, 32(1), 73–85. doi:10.1007/s10067-012-2093-2
Kuhn, J. E., Dunn, W. R., Sanders, R., An, Q., Baumgarten, K. M., Bishop, J. Y., … Wright, R. W. (2013). Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. Journal of Shoulder and Elbow Surgery, 22(10), 1371–1379.
Kukkonen, J., Joukainen, A., Lehtinen, J., Mattila, K. T., Tuominen, E. K. J., Kauko, T., & Äärimaa, V. (2014). Treatment of non-traumatic rotator cuff tears. The Bone & Joint Journal, 96-B(1), 75–81.
Moosmayer S Lund G Seljom U, et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: A randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br. 2010;92(1):83–91.
Littlewood C Ashton J Chance-Larsen K May S Ben Sturrock. Exercise for rotator cuff tendinopathy: a systematic review. Physiotherapy. 2012;98(2):101–109. [PubMed] [Google Scholar]
Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604.
Edwards P, Ebert J, Joss B, Bhabra G, Ackland T, Wang A.. Exercise rehabilitation in the non-operative management of rotator cuff tears: a review of the literature. Int J Sports Phys Ther. 2016;11(2):279–301. [PMC free article] [PubMed] [Google Scholar]
Björnsson HC Norlin R Johansson K Adolfsson LE. The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears: structural and clinical outcomes after repair of 42 shoulders. Acta Orthop. 2011;82(2):187–192. [PMC free article] [PubMed] [Google Scholar]
Smedbråten, K., Øiestad, B. E., & Røe, Y. (2018). Emotional distress was associated with persistent shoulder pain after physiotherapy: a prospective cohort study. BMC Musculoskeletal Disorders, 19(1). doi:10.1186/s12891-018-2142-3
Lewis J, McCreesh K, Roy J-S, et al. . Rotator cuff tendinopathy: Navigating the Diagnosis-Management conundrum. J Orthop Sports Phys Ther 2015;45:923–37. 10.2519/jospt.2015.5941 [PubMed] [CrossRef] [Google Scholar]
Ingwersen KG, Jensen SL, Sørensen L, Jørgensen HR, Christensen R, Søgaard K, et al. Three months of progressive high-load versus traditional low-load strength training among patients with rotator cuff tendinopathy: primary results from the double-blind randomized controlled RoCTEx trial. Orthop J Sports Med. 2017;5:2325967117723292. doi: 10.1177/2325967117723292. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211–220. [PMC free article] [PubMed] [Google Scholar]
Lai J., Gagnier J.J. The effect of lipid disorders on the risk of rotator cuff disease: A systematic review and meta-analysis. JBJS Open Access. 2018;3:e0018. doi: 10.2106/JBJS.OA.18.00018. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Nho SJ, Brown BS, Lyman S, et al. Prospective analysis of arthroscopic rotator cuff repair: Prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg 2009;18:13-20. [PubMed] [Google Scholar]
Collin P, Abdullah A, Kherad O, Gain S, Denard PJ, Lädermann A. Prospective evaluation of clinical and radiologic factors predicting return to activity within 6 months after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2015;24:439–445. [PubMed] [Google Scholar]
Novoa‐Boldo A, Gulotta LV. Expectations following rotator cuff surgery. Current Reviews in Musculoskeletal Medicine 2018; 11: 162–6. [PMC free article] [PubMed] [Google Scholar]
Russell, R. D., Knight, J. R., Mulligan, E., & Khazzam, M. S. (2014). Structural Integrity After Rotator Cuff Repair Does Not Correlate with Patient Function and Pain. The Journal of Bone & Joint Surgery, 96(4), 265–271.
Pappas, G. P., Blemker, S. S., Beaulieu, C. F., McAdams, T. R., Whalen, S. T., & Gold, G. E. (2006). In vivo anatomy of the Neer and Hawkins sign positions for shoulder impingement. Journal of Shoulder and Elbow Surgery, 15(1), 40–49. doi:10.1016/j.jse.2005.04.007
Leschinger, T., Wallraff, C., Müller, D., Hackenbroch, M., Bovenschulte, H., & Siewe, J. (2017). In vivo analysis of coracoid and subacromial shoulder impingement mechanism during clinical examination. European Journal of Orthopaedic Surgery & Traumatology, 27(3), 367–372.
Leschinger, T., Wallraff, C., Müller, D., Hackenbroch, M., Bovenschulte, H., & Siewe, J. (2017). Internal Impingement of the Shoulder: A Risk of False Positive Test Outcomes in External Impingement Tests? BioMed Research International, 2017, 1–5.
Kim, T. K., & McFarland, E. G. (2004). Internal Impingement of the Shoulder in Flexion. Clinical Orthopaedics and Related Research, 421, 112–119.
Klouche, S., Lefevre, N., Herman, S., Gerometta, A., & Bohu, Y. (2015). Return to Sport After Rotator Cuff Tear Repair. The American Journal of Sports Medicine, 44(7), 1877–1887.
Carbone, S., Candela, V., & Gumina, S. (2020). High Rate of Return to CrossFit Training After Arthroscopic Management of Rotator Cuff Tear. Orthopaedic Journal of Sports Medicine
Azzam, M. G., Dugas, J. R., Andrews, J. R., Goldstein, S. R., Emblom, B. A., & Cain, E. L. (2018). Rotator Cuff Repair in Adolescent Athletes. The American Journal of Sports Medicine, 46(5), 1084–1090.
Andrade R, Correia AL, Nunes J, Xará-Leite F, Calvo E, Espregueira-Mendes J, Sevivas N. Is Bony Morphology and Morphometry Associated With Degenerative Full-Thickness Rotator Cuff Tears? A Systematic Review and Meta-analysis. Arthroscopy. 2019 Dec;35(12):3304-3315.e2. doi: 10.1016/j.arthro.2019.07.005. PMID: 31785763.
Morelli KM, Martin BR, Charakla FH, Durmisevic A, Warren GL. Acromion morphology and prevalence of rotator cuff tear: A systematic review and meta-analysis. Clin Anat. 2019 Jan;32(1):122-130. doi: 10.1002/ca.23309. PMID: 30362636.
Bernstorff MA, Schumann N, Schwake L, Somberg O, Balke M, Schildhauer T, Königshausen M. Shoulder pathologies in CrossFit: a magnetic resonance imaging study of 51 cases. J Sports Med Phys Fitness. 2024 Mar 6. doi: 10.23736/S0022-4707.24.15071-2. Epub ahead of print. PMID: 38445843.
Weng PW, Chang WP. Influence of body mass index on severity of rotator cuff tears. J Shoulder Elbow Surg. 2024 Mar;33(3):648-656. doi: 10.1016/j.jse.2023.07.007. Epub 2023 Oct 31. PMID: 37573933.
Gumina S, Candela V, Passaretti D, Latino G, Venditto T, Mariani L, Santilli V. The association between body fat and rotator cuff tear: the influence on rotator cuff tear sizes. J Shoulder Elbow Surg. 2014 Nov;23(11):1669-74. doi: 10.1016/j.jse.2014.03.016. Epub 2014 Jun 4. PMID: 24906904.
Lawrence RL, Schlangen DM, Schneider KA, Schoenecker J, Senger AL, Starr WC, Staker JL, Ellermann JM, Braman JP, Ludewig PM. Effect of glenohumeral elevation on subacromial supraspinatus compression risk during simulated reaching. J Orthop Res. 2017 Oct;35(10):2329-2337. doi: 10.1002/jor.23515. Epub 2017 Mar 27. PMID: 28071815; PMCID: PMC5503805.
Giphart JE, van der Meijden OA, Millett PJ. The effects of arm elevation on the 3-dimensional acromiohumeral distance: a biplane fluoroscopy study with normative data. J Shoulder Elbow Surg. 2012 Nov;21(11):1593-600. doi: 10.1016/j.jse.2011.11.023. Epub 2012 Feb 22. PMID: 22361718.
Paavola M, Malmivaara A, Taimela S, Kanto K, Inkinen J, Kalske J, Sinisaari I, Savolainen V, Ranstam J, Järvinen TLN; Finnish Subacromial Impingement Arthroscopy Controlled Trial (FIMPACT) Investigators. Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: randomised, placebo surgery controlled clinical trial. BMJ. 2018 Jul 19;362:k2860. doi: 10.1136/bmj.k2860. PMID: 30026230; PMCID: PMC6052435.
Lawrence RL, Soliman SB, Roseni K, Zauel R, Bey MJ. In vivo evaluation of rotator cuff internal impingement during scapular plane abduction in asymptomatic individuals. J Orthop Res. 2023 Apr;41(4):718-726. doi: 10.1002/jor.25423. Epub 2022 Sep 6. PMID: 35880416; PMCID: PMC9877247.
Adding Manual Therapy to an Exercise Program Improves Long-Term Patient Outcomes Over Exercise Alone in Patients With Subacromial Shoulder Pain: A Randomized Clinical Trial Lori A. Michener, Philip W. McClure, Angela R. Tate, Lane B. Bailey, Amee L. Seitz, Rachel K. Straub, and Charles A. Thigpen JOSPT Open 2024 2:1, 29-48
Paraskevopoulos E, Plakoutsis G, Chronopoulos E, Maria P. Effectiveness of Combined Program of Manual Therapy and Exercise Vs Exercise Only in Patients With Rotator Cuff-related Shoulder Pain: A Systematic Review and Meta-analysis. Sports Health. 2023 Sep-Oct;15(5):727-735. doi: 10.1177/19417381221136104. Epub 2022 Dec 14. PMID: 36517977; PMCID: PMC10467476.
Pieters L, Lewis J, Kuppens K, Jochems J, Bruijstens T, Joossens L, Struyf F. An Update of Systematic Reviews Examining the Effectiveness of Conservative Physical Therapy Interventions for Subacromial Shoulder Pain. J Orthop Sports Phys Ther. 2020 Mar;50(3):131-141. doi: 10.2519/jospt.2020.8498. Epub 2019 Nov 15. PMID: 31726927.
Flowers DW, Swanson BT, Shaffer SM, Clewley DJ, Riley SP. Is there 'trustworthy' evidence for using manual therapy to treat patients with shoulder dysfunction?: A systematic review. PLoS One. 2024 Jan 18;19(1):e0297234. doi: 10.1371/journal.pone.0297234. PMID: 38236928; PMCID: PMC10796022.
Schydlowsky P, Szkudlarek M, Madsen OR. Comprehensive supervised heavy training program versus home training regimen in patients with subacromial impingement syndrome: a randomized trial. BMC Musculoskelet Disord. 2022 Jan 15;23(1):52. doi: 10.1186/s12891-021-04969-0. PMID: 35033043; PMCID: PMC8760780.
Dubé MO, Desmeules F, Lewis JS, Roy JS. Does the addition of motor control or strengthening exercises to education result in better outcomes for rotator cuff-related shoulder pain? A multiarm randomised controlled trial. Br J Sports Med. 2023 Apr;57(8):457-463. doi: 10.1136/bjsports-2021-105027. Epub 2023 Feb 16. PMID: 36796859.
Hopewell S, Keene DJ, Heine P, Marian IR, Dritsaki M, Cureton L, Dutton SJ, Dakin H, Carr A, Hamilton W, Hansen Z, Jaggi A, Littlewood C, Barker K, Gray A, Lamb SE. Progressive exercise compared with best-practice advice, with or without corticosteroid injection, for rotator cuff disorders: the GRASP factorial RCT. Health Technol Assess. 2021 Aug;25(48):1-158. doi: 10.3310/hta25480. Erratum in: Health Technol Assess. 2022 Aug;25(48):159-160. PMID: 34382931; PMCID: PMC9421560.
Fatima A, Ahmad A, Gilani SA, Darain H, Kazmi S, Hanif K. Effects of High-Energy Extracorporeal Shockwave Therapy on Pain, Functional Disability, Quality of Life, and Ultrasonographic Changes in Patients with Calcified Rotator Cuff Tendinopathy. Biomed Res Int. 2022 Mar 4;2022:1230857. doi: 10.1155/2022/1230857. PMID: 35281612; PMCID: PMC8916860.
Robinson DM, Eng C, Makovitch S, Rothenberg JB, DeLuca S, Douglas S, Civitarese D, Borg-Stein J. Non-operative orthobiologic use for rotator cuff disorders and glenohumeral osteoarthritis: A systematic review. J Back Musculoskelet Rehabil. 2021;34(1):17-32. doi: 10.3233/BMR-201844. PMID: 33361581.
Sari A, Eroglu A. Comparison of ultrasound-guided platelet-rich plasma, prolotherapy, and corticosteroid injections in rotator cuff lesions. J Back Musculoskelet Rehabil. 2020;33(3):387-396. doi: 10.3233/BMR-191519. PMID: 31743987.
Schoch BS, Werner BC, Shapiro SA, Camp CL, Chalmers PN, Cancienne JM. Effect of Bone Marrow Aspirate Concentrate and Platelet-Rich Plasma Augmentation on the Rate of Revision Rotator Cuff Repair. Orthop J Sports Med. 2022 Nov 3;10(11):23259671221127004. doi: 10.1177/23259671221127004. PMID: 36353396; PMCID: PMC9638537.
Khan AZ, Stoll KE, Erickson BJ. Rehabilitation and Return to Work and Sport After Rotator Cuff. Clin Sports Med. 2023 Jan;42(1):175-184. doi: 10.1016/j.csm.2022.08.008. PMID: 36375868.
Longo UG, Risi Ambrogioni L, Candela V, Berton A, Carnevale A, Schena E, Denaro V. Conservative versus surgical management for patients with rotator cuff tears: a systematic review and META-analysis. BMC Musculoskelet Disord. 2021 Jan 8;22(1):50. doi: 10.1186/s12891-020-03872-4. Erratum in: BMC Musculoskelet Disord. 2021 Sep 2;22(1):752. PMID: 33419401; PMCID: PMC7796609.
Dubé MO, Desmeules F, Lewis J, Roy JS. Rotator cuff-related shoulder pain: does the type of exercise influence the outcomes? Protocol of a randomised controlled trial. BMJ Open. 2020 Nov 5;10(11):e039976. doi: 10.1136/bmjopen-2020-039976. PMID: 33154058; PMCID: PMC7646354.
Puzzitiello RN, Patel BH, Nwachukwu BU, Allen AA, Forsythe B, Salzler MJ. Adverse Impact of Corticosteroid Injection on Rotator Cuff Tendon Health and Repair: A Systematic Review. Arthroscopy. 2020 May;36(5):1468-1475. doi: 10.1016/j.arthro.2019.12.006. Epub 2019 Dec 17. PMID: 31862292.
Lin CY, Huang SC, Tzou SJ, Yin CH, Chen JS, Chen YS, Chang ST. A Positive Correlation between Steroid Injections and Cuff Tendon Tears: A Cohort Study Using a Clinical Database. Int J Environ Res Public Health. 2022 Apr 8;19(8):4520. doi: 10.3390/ijerph19084520. PMID: 35457390; PMCID: PMC9031762.
Giovannetti de Sanctis E, Franceschetti E, De Dona F, Palumbo A, Paciotti M, Franceschi F. The Efficacy of Injections for Partial Rotator Cuff Tears: A Systematic Review. J Clin Med. 2020 Dec 25;10(1):51. doi: 10.3390/jcm10010051. PMID: 33375716; PMCID: PMC7795404.
Sciascia A, Kibler WB. Current Views of Scapular Dyskinesis and its Possible Clinical Relevance. Int J Sports Phys Ther. 2022 Feb 2;17(2):117-130. doi: 10.26603/001c.31727. PMID: 35136680; PMCID: PMC8805107.
———————————————————————–













